Denial Management Software
When a healthcare patient’s insurance claim for treatment gets denied by their health insurance company, it causes a headache and stress not only for that patient—but also for the practice or hospital that provided care. When insurance companies deny claims, treatment providers risk not getting paid for the services and care they have provided. Hospitals may also not receive funds to cover supplies and medication they used.
Because the denial of health insurance claims can be costly, healthcare organizations have put a lot of money and resources into honing denial management solutions — or coming up with ways to handle a denied insurance claim so that practices get paid, and patients aren’t hit with unexpected and unmanageable bills.
Until recently, the problem with denial management efforts has been that they have centered on the backend or “revenue cycle” of a hospital — long after patients have received care and been discharged. Leaving denial management solely in the hands of hospital revenue cycle and utilization review teams means tackling the problem of denied claims long after admissions decisions have already been made (correctly or incorrectly). Usually, patients are long gone from a hospital. In other words, this is an attempt to fix a problem retroactively when a preventative approach actually makes more sense.
There are more effective ways to handle denial management—especially if they are focused on prevention. Putting the process in the hands of physicians at the time an admission decision must be made (rather than in the billing department’s hands after claims have already been denied) helps decrease the likelihood that a health insurance company will deny any claim in the first place and in turn, prevent any claim denial issues before they ever occur.
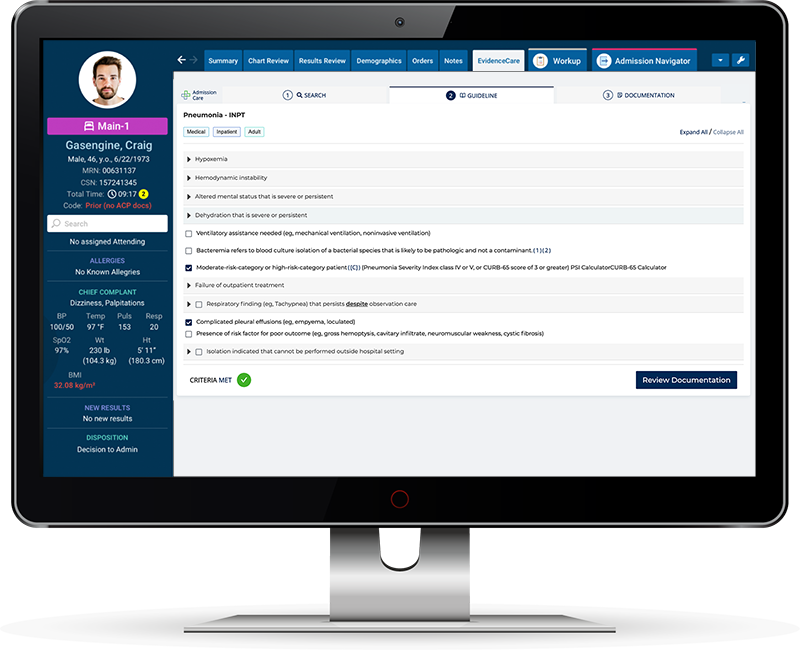
One tool that enables this new approach is a healthcare denial management software solution called AdmissionCare. AdmissionCare reduces denials by giving physicians the appropriate bed status decision at the time of hospital admission.
While AdmissionCare is not what people typically think of today when looking for a denial management solution they can use (i.e. programs billing teams can use once an insurance company has denied a claim), it is actually an incredibly useful resource because it reduces the likelihood that any treatment decision will get denied by health insurance payers in the first place, and that neither hospital nor patient will have to stress over the prospect of an unpaid or unpayable bill.
When searching for hospital denial management software, many are focusing on the issue from a revenue cycle or utilization review perspective. However, AdmissionCare is an example of denials management software that is changing the status quo by taking the some of the burden for managing claim denials out of the hands of people focused on the revenue cycle and equipping physicians or clinicians who can correct the problem at the source.
What is Denial Management In Healthcare?
Denials in healthcare are extremely common. A recent study released by the Kaiser Family Foundation showed that in the last two years, on average, 18% of all in-network healthcare claims were denied by health plans sold on the federal health insurance marketplace. However, the denial rate of some plans was as high as 80%. And experts believe this is a problem that is only getting worse — not better — and that claim denials are going to continue to increase in the coming years.
Thus, healthcare denial management is a critical part of the medical care process. When claims are denied, hospitals and medical practices experience a loss or delay of billions of dollars of reimbursements, which can affect their ability to operate properly. So, denial management in healthcare is the means by which providers can recoup the money spent on providing patient care, and patients can figure out a way to navigate large medical bills that they cannot afford on their own.
Despite its importance, denial management in healthcare has been largely ineffective. Typically, when a healthcare denial happens, the billing department at a practice or hospital is informed, along with a reason behind the denial. The team in charge of denials management, in turn, reviews the claim and reason for denial carefully, determines whether it can be contested, and then fixes whatever error caused the denial.
Research shows that 40% of denied claims are caused by issues with medical necessity, authorizations, precertifications, medical documentation, or service coverage. Medical practice staff can miss details in a patient’s insurance plan, including the exclusion of specific services or the need for prior authorizations or referrals.
When an error in a claim has been identified and corrected, the healthcare denials management team can resubmit the claim. If a resubmitted claim is denied again, the process can be appealed by submitting an explanation of your reason behind the appeal to the insurance provider, as well as all documentation that supports your claim.
Currently, this manual review and appeal process is long and unwieldy. It leaves the responsibility of reversing a claim denial decision in the hands of an administrative team, who must comb through plan information and patient records to spot errors that were made at the time of admission — a time when they were not involved in or informed about the patient’s care.
Hospital Denials Management
Claim denials are a problem throughout the entire healthcare industry, but they are particularly challenging in a hospital setting. The reason for this is that many patients enter a hospital in the emergency department, and physicians must make fast decisions about a patient’s bed status.
A hospital bed status decision happens when a physician must decide whether a patient should be kept in the ED for observation or whether they should be admitted for inpatient care. ED doctors must make admissions decisions in a fast-paced, high-pressure environment based on a variety of factors (including the needs of the patient, the type of care that insurance plans will most likely cover, and more).
Right now, most physicians and care providers make these decisions based on past experience or intuition without having facts and evidence-based criteria on hand. And while physicians are almost always well-meaning in their decision-making process, wanting to offer the best care to patients and choose an appropriate course of treatment an insurance plan will cover, most are not well-versed in or privy to all of the intricacies of the many insurance plans available today. Thus, they are not informed about what a patient’s health insurance plan requires to ensure treatments are covered, and the process results in many bed status denials once insurance companies receive claims.
Hospital admission decision denials are costly for hospitals and can limit or stop their cash flow. They also almost always happen after patients have received their care and been discharged when money is already owed for services and supplies provided.
When insurance companies refuse to pay for costly treatments, billing departments or hospital denials management teams must spend time determining why the claim was denied and then retroactively take administrative steps to try to get those claims approved, which can be time-consuming, tedious, and require several attempts in order to be successful. If the attempt to correct a claim is still denied, hospitals can appeal decisions, but the appeals process can be a lengthy battle that both costs the hospital money and draws out the time frame during which they could potentially get paid for the care.
The good news in the world of hospital denials management is that many of these denials can be fixed by getting medical necessity documentation right at the source. Thus, reducing denials can be an easy process — if you take denial management out of the hands of people who handle the hospital revenue cycle retroactively and put it into the hands of the physicians making bed status decisions. Hospital denial management best practices show that it is incomparably more effective to take preventative steps to avoid claim denials—not try to fix them in retrospect.
Denial Management Workflow
To reverse the problem of increasing claim denials in hospital settings, emergency room physicians need to have evidence-based criteria in their hands before making bed status decisions. One way to give them the information they need is by ensuring they have bed status criteria in their EHR, so they can quickly add the documentation needed for a patient to be admitted or placed in observation status. Using a prevention-centered denial management workflow stops denials before they ever happen.
Thankfully there is software today that make it easier than ever for ED doctors to access the data they need in real-time to make informed decisions. AdmissionCare is a software created with physicians in mind. It arms physicians with the criteria they need in their EHR to transform the clinical decision-making process. By introducing a tool that changes the denial management workflow, hospitals can reduce the chances they have denials in the first place, improve their revenue streams and reimbursement rates with no bottlenecks, and ensure that patients get the care they need and deserve without hesitation.
Want to learn more about EvidenceCare’s denial management software, AdmissionCare?
Schedule a demo today.