Denial Management in Healthcare
Denial management in healthcare is the process by healthcare organizations to handle denied claims from medical insurance payers. Medicare, Medicaid, commercial health insurers, and third-party payers often deny a percentage of claims submitted for medical services.
So, what are the denial codes? The most common denial codes in medical billing include invalid procedure codes, non-covered services, coding errors, scope of license issues, and experimental/investigational procedures.
Here are the medical billing denial codes and reasons:
-
- Invalid procedure code: The procedure code billed does not match the service provided.
- Scope of license: The procedure was performed by a provider not licensed or certified to perform that service.
- Coding error: An incorrect procedure or diagnosis code was used.
- Non-covered service: The billed service is not covered under the patient’s insurance plan or health benefits.
- Experimental/investigational procedure: The treatment is considered experimental or investigational and is not covered.
- Patient’s condition: The procedure was medically unnecessary for the patient’s condition or illness.
It is, therefore, important for healthcare facilities to have a process in place for denial management. Effective denial management involves thoroughly reviewing all denial codes and reasons, determining if an appeal is warranted, and submitting corrected or additional documentation to appeal the denial. Many healthcare providers can overturn a significant percentage of denials through appeals.
Denied claims in healthcare represent lost revenue that providers need to recoup to remain financially viable. A pattern of denied claims that remain unappealed or unsuccessful in appeal represent a significant threat to healthcare operations and profitability.
Providers must focus on educating staff, auditing claims, and appealing these frequently denied procedures and service codes. With diligent denial management, healthcare providers can minimize revenue loss and maximize reimbursement for medically necessary patient services. Effective denial management is crucial to success in today’s healthcare economy.
Denial Management Process
An effective denial management process is key to reducing claim denials and ensuring optimal revenue recovery in healthcare organizations. Providers can systematically review and appeal denied claims by implementing a structured denial management workflow to overturn more denials and increase reimbursement.
Developing a denial management & appeals reference guide helps standardize the process and ensures consistency across reviewers. This guide should reference essential resources like the Medicare denial reason codes manual to properly interpret denial codes and determine the most compelling arguments for each appeal.
The core steps of a denial management process in healthcare include the following:
-
- Identify denied claims – Regularly run reports to pull all denied claims and identify potentially appealable denials. Review denial reason codes and documentation to determine the merit of the appeal.
- Gather additional documentation – For strong appeals, obtain any missing information or clarifications needed to resubmit the claim. This could include charts, test results, prescriptions, etc.
- Draft appeal letter – Write a formal appeal letter addressing the specific reason for denial and including any additional supporting documentation. The letter should be persuasive but professional.
- Submit appeal – Submit the appeal through the proper channels, whether in writing, electronically, or via phone. Follow up regularly to ensure there is no delay in processing the appeal.
- Monitor appeal status – Track the status of each appeal submission and follow up again if there is no decision within the required timeframes to avoid missing opportunities for overturning denials.
- Analyze and improve – Regularly review the outcome of appealed claims to determine which denial reasons and issues are most frequently overturned. Use these insights to refine and improve the denial management process to achieve higher and higher denial overturn rates over time.
Healthcare organizations implementing an efficient denial management process can optimize revenue, reduce costs, and ensure the highest quality and compliance. An evidence-based appeals strategy is key to appealing denials successfully at scale.
Types Of Denials
A denial in healthcare means that an insurance company will not cover part or all of the costs associated with a medical claim. There are several types of denials healthcare providers encounter.
Rejection
Healthcare denial can span from rejecting an entire claim to just portions of the claim. The difference between a rejection and denial in medical billing is that a rejection means no part of the claim is approved and payment is not issued. On the other hand, a denial means at least some portion of the claim is approved and paid.
Hard Denial
Hard denials in medical billing refer to denials where the insurance company will not budge on their decision. These prove difficult to overturn and appeal. It is helpful for providers to understand the list of denial codes in medical billing used by insurers in determining reasons for denials.
Medical Necessity Denial
Medical necessity denials involve situations when the care provided was deemed not medically necessary according to the insurer’s guidelines. Appeals often require more clinical documentation to justify medical needs.
Insurance companies will have internal appeals procedures and the option to pursue external independent reviews. Multiple levels of appeal may be needed, including filing grievances with state insurance regulators regarding inappropriate denial decisions. In some situations, obtaining legal counsel to review the improper denial of medically necessary care is advisable.
While navigating the denial and appeals process can be challenging, keeping exhaustive records of all communications, denied claims, submitted appeals evidence, and outcomes at each stage is critical. Detailed records help establish a comprehensive case demonstrating medical necessity and provide evidence if further legal action is contemplated.
Technical Denial
A technical denial in healthcare refers to a denial issued due to a mistake, omission, or error on the claim form submission, like missing information, incorrect codes, etc. These denials can often be appealed and resubmitted with the proper corrections and documentation.
Other hospital denials include denials for non-covered procedures, exhausted benefits, cosmetic procedures, and experimental treatments.
Knowing the potential types of denials, denial codes list, and appeals process can help healthcare providers work to overturn inappropriate denials and ensure proper reimbursement for services rendered.
Staying up-to-date on all contracted insurers’ policies, guidelines, and benchmarks also helps minimize denials whenever possible. With effective denial management, providers can improve cash flow and maintain positive relationships with payers.
Preventing Denials in the Hospital
Denial management workflows have become increasingly important for hospitals and healthcare systems. Administrators need staff experienced in denial management in medical billing to lower claim denial rates and ensure proper reimbursement.
Handling medical claim denials effectively is critical for any hospital’s financial well-being. Preventing denials in the hospital should be a top priority to avoid lost revenue and increased costs. Some key strategies for hospital denial management include:
-
- Automate denials management: Using automated software tools to sort, process, and adjudicate denials helps streamline the workload and promptly address denials. Hospitals can automate denial management and significantly reduce manual tasks.
- Implement targeted audits: Regular audits of high-deny categories like emergency room claims can uncover specific issues to target education or process improvements. Audits also provide an extra check to avoid human errors.
- Provide robust education: Ensuring all staff involved in the billing lifecycle understand coverage guidelines, coding rules, and proper documentation is essential. Ongoing education and training help minimize accidental errors.
- Enhance documentation practices: Strengthening documentation at every stage of care, from intake to discharge, builds a comprehensive record to support medical necessity, and correctly coded claims.
- Collaborate across departments: Bringing together teams from coding, billing, compliance, and medical staff fosters a shared understanding of issues and opportunities. Cross-collaboration leads to innovative solutions.
- Build advocacy support: When denial issues stem from policy or coverage disputes, provider advocacy through medical director oversight and appeals can successfully negotiate with payers on hospitals’ behalf.
With a robust denial management program, hospitals can gain revenue, reduce costs, improve payer relationships, and enhance overall financial health. Effective denial management is crucial to overcoming threats and capitalizing on opportunities in today’s healthcare landscape.
Denial Management Software
Managing insurance claims denials is an ongoing challenge for providers and health organizations. According to studies, up to 15 – 17% of medical claims result in some level of denial, costing the healthcare industry over $48.3 million annually in administrative fees and lost revenue.
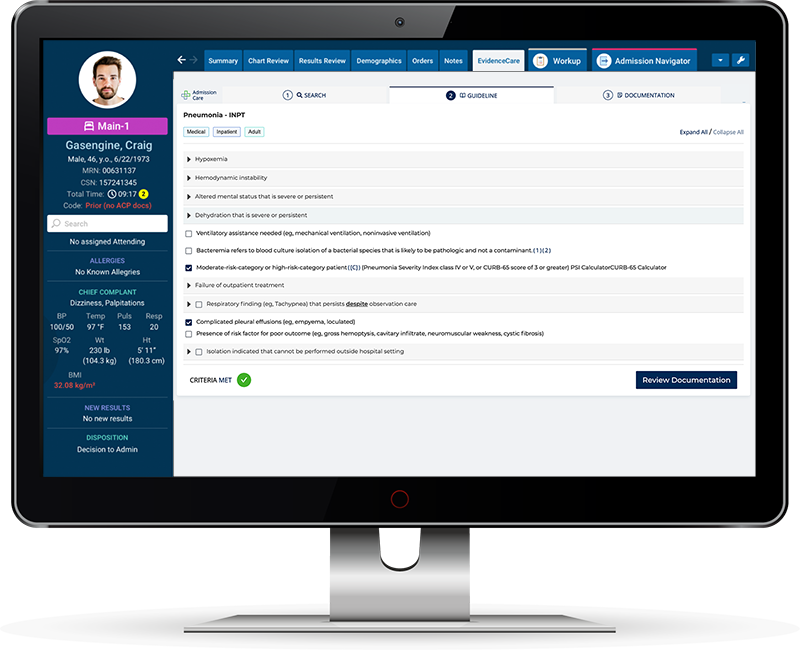
The solution is implementing denial management software and leveraging a denial management solution that starts by empowering the ones delivering care – physicians. When medical necessity denials occur, it’s often because of documentation. Software can help doctors get this info right at the source to minimize revenue leakage and ensure faster payment.
AdmissionCare is the leading denial management software and is considered the best tool for this work. The EHR-integrated solution helps reduce claim denials by putting the criteria for hospital admission in the physician’s workflow that automatically creates the proper documentation in the medical record. AdmissionCare utilizes criteria and guidelines that payers use – such as MCG and Interqual – to determine the documentation needed to avoid the top reasons for denials so providers can get it right at the source.
Providers can proactively manage the denial process using EHR-integrated denial management software in addition to systematic policies, workflows, reporting, and tracking. Some of the key benefits of using this software include:
-
- Improved cash flow: The faster resolution of denied claims means quicker payment and reduced Days in Accounts Receivable (DIR).
- Happier Clinicians: Admitting physicians, hospitalists, and UR teams are better aligned and interrupt each other less with proper documentation
- Cost containment: Less administrative time and costs are incurred by preventing future denials and having medical necessity documented for inpatient admissions — increasing profit margins.
- Actionable insights: Reporting analytics provide visibility into denial rates, reasons, insurers, and opportunities to optimize processes. Data can drive performance improvement initiatives.
Reducing claim denials is an ongoing challenge. However, with the right denial management solution and software like AdmissionCare by EvidenceCare, the healthcare industry can overcome hurdles, improve financial outcomes, and focus resources on patient care. The adoption of denial management tools is critical to sustaining long-term business success.
Schedule a demo of AdmissionCare today!