Importance of Documentation in Healthcare
Documentation in the healthcare industry is not just nice to have, it’s a necessity.
The importance of documentation in healthcare directly relates to the quality of patient care. It would be impossible to provide exceptional patient care without proper documentation of the patient’s current and past medical history. It also has a major impact on billing, insurance, and the finances of both the hospital and patient.
While nearly all medical professionals understand the importance of documentation in the medical industry, the process of keeping medical records accurate and up to date can be cumbersome, to say the least.
Value of EHR Software
The HITECH Act of 2009 requires medical providers to maintain up-to-date Electronic Medical Records (EMR). This act helps streamline the medical documentation process and makes it easier for healthcare providers and systems to share information with each other and their patients.
Today, most healthcare systems use Electronic Health Record (EHR) software to maintain proper documentation in healthcare. This software can help improve the efficiency of maintaining medical records but also puts doctors in a position to make insurance-based decisions that they may not fully understand.
For example, emergency room doctors often determine bed statuses for patients – are they inpatient or just there for observation? While the medical decision for the doctor may be clear, unfortunately, there’s a lot of ambiguity regarding the guidelines for bed status determinations.
As a result, physicians are prone to select the less restrictive bed status – observation. This may seem like a small thing, but the wrong determination can have significant ramifications, including lower quality of patient care and lost revenue for the hospital.
Medical providers must focus not only on the importance of documentation in the hospital, but also on making the documentation process as easy as possible for physicians who are not trained in medical billing. This article provides more information about the importance of medical records in hospitals and other medical facilities and how hospital admissions documentation improvement software can help.
3 Main Reasons Documentation Is Important in Healthcare
Documentation in the healthcare industry is important for doctors, nurses, and healthcare facilities.
Why Is Documentation Important for Doctors?
Physicians see many patients on a regular basis. It would be impossible to track each patient’s medical history without proper documentation.
Doctors rely on this documentation, whether it’s from the services they provide, test results, nurses’ input, or data from other medical professionals when making healthcare decisions, diagnoses, and treatment plans for patients.
Why Is Documentation Important in Nursing?
Proper documentation improves communication between doctors and nurses. Rather than relying on memory, nurses can use EHR software to see exactly what the doctor’s orders are.
It also allows nurses to relay to doctors the patients’ vital signs, any additional symptoms or issues, and what treatment and services have been provided.
Why Is Documentation Important in Healthcare?
The three main reasons documentation is important in healthcare include:
1. Improved Quality of Patient Care
The most important benefit of documentation in healthcare is that it can improve the quality of patient care. When doctors have the patient’s complete medical history in front of them, they can make better decisions regarding diagnosis and treatment.
2. Enhanced Communication
The importance of electronic health records is undeniable.
It not only improves communication between medical providers but also gives patients greater access to their own medical records. This enhanced communication can reduce the risk of medical errors and improve patient outcomes.
3. Increased Claim Approval Rates
Documenting services at the point of care can reduce the risk of errors and increase medical claim approval rates. This results in greater profits for healthcare providers and lower out-of-pocket expenses for the patient.
Hospital Admission Documentation
Documentation is an important process in all areas of healthcare, including hospital admissions. Hospitals, especially emergency rooms, can sometimes be chaotic, and accurate documentation is critical.
When a patient comes to the hospital, doctors must determine the patient’s bed status. For instance, is the patient being admitted to the hospital or simply there for observation?
In some scenarios, making this determination is clear-cut. For example, if the patient requires inpatient surgery, they will be admitted to the hospital.
Other times, making this determination is not so easy.
Either way, doctors must make decisions using bed status criteria when patients are admitted to the hospital. For insurance companies to successfully process these claims, doctors must also provide bed status documentation that shows why they made their determination.
Claim denials are becoming increasingly common due to incorrect status claims. This is primarily due to the fact that it’s difficult for doctors to make these bed status determinations for several reasons, including:
-
- Doctors are trained to provide medical care to patients, not in the complexities of medical billing.
- Emergency room care often evolves and changes as doctors gather more data and test results.
- Guidelines pertaining to hospital admission criteria can be complex, ambiguous, and constantly changing.
These factors highlight the importance of accurate documentation, especially in critical and emergency nursing care.
While EHR software makes storing and maintaining medical records easier, it typically does very little to help doctors make accurate bed status decisions or ensure the appropriate hospital admission documentation is completed. The software prompts doctors to input specific information, but in many cases, this type of software doesn’t provide the guidance physicians need to make accurate determinations at the point of care.
Medical Documentation Guidelines
Medical documentation guidelines provide detailed information about what forms and documents insurance providers need to process a claim. If only one piece of information is missing from the claim, the healthcare insurance company may deny it and fail to reimburse the hospital.
When a denial happens, the healthcare provider must fill in the missing data and track down the missing medical record documentation before resubmitting the claim. This process wastes both time and money – and with no guarantee the claim will be approved the second time around. In fact, entire departments and outsourced companies exist to help revenue cycle and utilization management teams with this denial management process.
Perhaps if there were only one set of medical documentation guidelines that medical providers had to follow, the process would be easier. But this is not the case.
Instead, doctors must understand various guidelines, including:
Unfortunately, these guidelines can be complex and vague for clinicians focused on medical practice, which only leads to more confusion and incorrect claims.
In order to reduce the risk of a claim denial, doctors must understand the hospital admission documentation requirements. For example, the Medicare two-midnight rule is especially vague.
Without appropriate documentation explaining why the patient requires this level of care, Medicare could deny the claim. This denial can decrease revenue for the hospital and shift the burden of payment onto the patient.
Many health systems rely on EHR software to prompt physicians to provide as much documentation as possible. This can be a good start, but if the software doesn’t guide doctors through the admission process by using evidence-based guidelines, it may not be enough.
For example, doctors can’t simply list the patient’s symptoms and diagnosis, and hope the insurance company can figure it out. Instead, they must provide documented proof of why the patient required the level of care selected.
Hospital Admissions Documentation Improvement Software
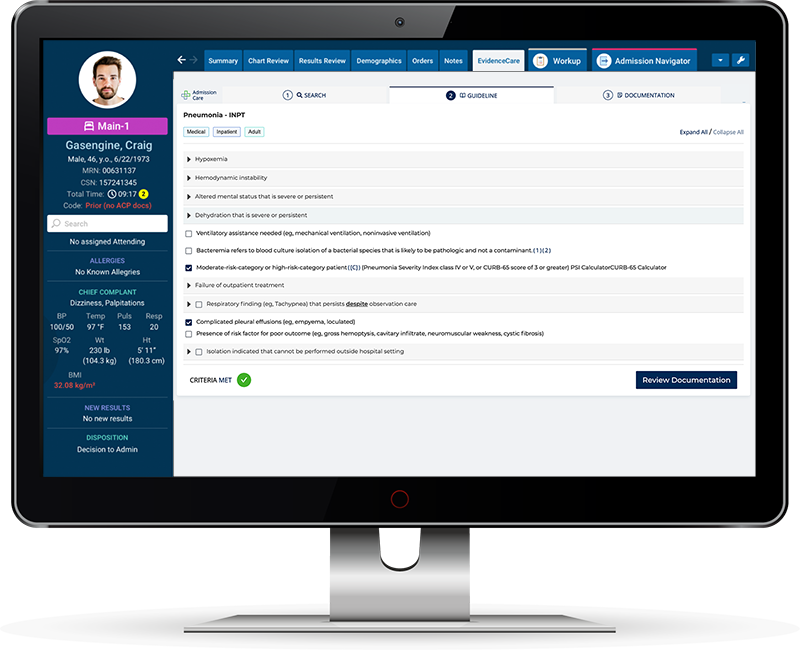
To overcome the challenges of claim denials, inaccurate bed status determinations, and lack of documentation, many hospitals are investing in clinical documentation improvement software, like AdmissionCare.
This software takes the stress out of making these determinations and securing the right documentation by integrating evidence-based guidelines directly into its EHR software. This software focuses on helping doctors make the right bed status determination, and backing up those decisions with corresponding documentation.
There are many benefits of using hospital admission documentation improvement software, such as:
1. Better Patient Care
Most importantly, hospital admission documentation improvement software can lead to better patient care. It allows doctors to spend less time trying to figure out complex insurance guidelines, and instead focus on providing care to the patient.
2. Improved Workflow
Utilization management software can improve emergency room workflow by significantly reducing the frustration and time it takes to complete the hospital admission process. It also improves communication between doctors, patients, and medical billing representatives.
3. Increased Patient Satisfaction
When patients can receive faster services, with fewer insurance issues, it can drastically improve patient satisfaction. Higher satisfaction will keep your patients coming back to your hospital if necessary, and refer your services to others.
4. Fewer Claim Denials
By focusing on utilization management documentation improvement strategies, the hospital can reduce the number of claim denials it receives. This, in turn, can improve hospital revenues, which it can then use to increase patient services.
5. Lower Out-of-Pocket Expense
When the insurance provider denies a claim, the burden of payment instantly shifts to the patient. In many cases, patients simply can’t afford to pay these higher out-of-pocket expenses. Using software to make accurate bed status decisions can reduce the risk of unnecessary out-of-pocket expenses.
Take steps now to improve how your hospital handles the admission and documentation process, by investing in clinical documentation improvement software like AdmissionCare.
Want to learn more about EvidenceCare’s clinical documentation software, AdmissionCare?
Schedule a demo today.