Criteria For Hospital Admission
ED clinicians, who do the initial assessment of patients for admission, are not taught in school the differences in emergency admission criteria such as, Outpatient/Observation status versus Inpatient status. They enter the workforce well-versed in what medically requires a hospital stay, but not necessarily the criteria for hospital admission.
It is the admitting physician who is ultimately responsible to determine the most appropriate status. He/she must also write the best, specific story on why he/she feels the patient needs to “buy a bed.” Unfortunately, when a patient is too sick to be sent home, the documentation of ‘how sick the patient is’ is important for the insurance company to approve the services given to the patient.
A healthcare insurance company has specific guidelines (MCG or InterQual) or proprietary standards for when to provide financial coverage for medically appropriate services. This is why it’s important to understand that an admission status is closely related to the acuity of the patient and is important when caring for a patient.
Through the years, hospitals have had to find ways to make sure patients are billed in their correct status to prevent billing patients incorrectly and prevent insurance denials. By developing a utilization management department staffed by nurses, hospitals have a way to evaluate medical necessity of healthcare services to determine which status is most appropriate for the patient. The issue is that nurses may not have the entire story related to the reason for admission and documentation does not support the acuity of service and therefore must contact the admitting provider to relay that information.
Having to determine if an insurance company will provide coverage, once the decision is made to admit a patient, requires understanding of these insurance guidelines or standards which is beyond what physicians are taught in their medical training. If a patient is placed in the wrong status, insurance companies can deny payment which means a hospital will not be reimbursed on the care given to the patient. This is a financial loss to the hospital and can potentially negatively impact the patient.
Hospital administrators manage facility finances and budgets to ensure their hospital remains fiscally sound and must comply with federal laws and regulations. Denied payments can put a hospital in a financially debilitating position and must rely on physician and UR teams to get the admission process right. Just like we all manage a budget at home or at work, hospital operators and clinicians must work together to keep hospitals in business.
If you want to know more about the criteria for hospital admission and the hospital admissions process, continue reading about why hospital admissions can be so complex, slow, and problematic and solutions to make it simpler.
Hospital Admission Documentation Requirements
While ED doctors are trained to provide care to patients, they also need to understand the administrative process of patient admissions. One key aspect of this is for doctors to be well-versed in hospital admission documentation requirements for patients with commercial insurance as well as Medicare and Medicaid — insurance coverage provided by the Centers for Medicare and Medicaid (CMS).
CMS provides health coverage to more than 100 million people throughout the United States. Many people who come to the ED have this publicly provided insurance. Because so many patients have CMS insurance, doctors are subjected to understanding the Medicare two midnight rule. This is what often guides their decision-making process when deciding to admit a patient or not: they must carefully assess whether the patient meets CMS’ criteria for admission of staying over 2 midnights to meet the acuity of inpatient status or if they need a brief, outpatient evaluation in observation services until they’re ready to go home.
The CMS two-midnight rule argues that patients should simply stay in observation unless the care they require will need to go on for two days or longer. What is crucial to this rule is that the documentation must show the acuity and support the patient requiring inpatient services.
Keeping a patient in a hospital bed for this time frame awaiting placement, further testing, or for patient convenience is not appropriate. This is CMS’ way of lowering unnecessary hospital admissions. CMS originally created this rule of how to avoid observation status due to patient complaints of staying in observation status too long, which caused financial hardship and not qualifying for a skilled nursing facility stay.
Inpatient Vs Observation Criteria
If a physician or admitting practitioner certifies that the patient will be in the hospital for at least two midnights, they are asking for pre-approval of payment from CMS for inpatient services. While intended to be a decision based only on an assessment of the patient’s medical needs, it also depends on additional non-clinical factors like expected length of stay and the specificity of documentation supporting the hospital inpatient claim. Observation services are for patients who cannot be sent home from the ED and are not sick enough for inpatient status or who need short term (less than 2 midnights) evaluation of their symptoms.
Utilization Review teams generally familiarize themselves with the patient guidelines for inpatient vs observation provided by MCG or Interqual, as well as the two-midnight rule that Medicare provides. The UR team can support patient status decisions, typically retrospectively, but physicians and admitting practitioners are ultimately responsible for this decision.
It is important to get this decision correct concurrently, and if the practitioner gets it right from the start, it eliminates issues in the future of having to defend yourself for your decisions.
Observation vs. inpatient reimbursements or payments to the hospital for services given differ significantly, so CMS wants hospitals to be sure that a patient really requires a hospital stay out of true medical necessity. The two-midnight rule is a tool that can help guide a doctors’ decisions regarding inpatient care (IP) vs observation (OBS) when admitting a patient from the ER, especially when the decision regarding admission vs. observation is not so clear-cut. But again, 2 MNs alone is not enough to ensure that care will be covered as ‘medical necessity’ or the ‘severity of the patient disease or symptoms’ require inpatient care.
On the physician billing side, the same Evaluation & Management (E&M) code will be used for observation or inpatient, but the place of service code must be correct. Starting in 2023 there will be initial admit E&M codes which different by decision making (low, moderate, or high). Subsequent day E&M codes also are based on low or high complexity only. The place of service code is either outpatient (observation) or inpatient.
Types Of Hospital Admission Criteria
There are a few different types of hospital admission criteria that physicians can use when it comes to making decisions about hospital admissions – observation admission criteria and inpatient admission criteria – essentially, whether patients should have outpatient/observation services or whether they qualify for admission to the hospital for, more acute services.
When it comes to the process of creating concrete guidelines for inpatient or observation criteria, there are two companies that have led the way: MCG criteria for hospital admission and InterQual criteria for hospital admission. They have both come up with evidence-based set of guidelines that physicians can use for gauging the most accurate patient status based on the patient’s acuity.
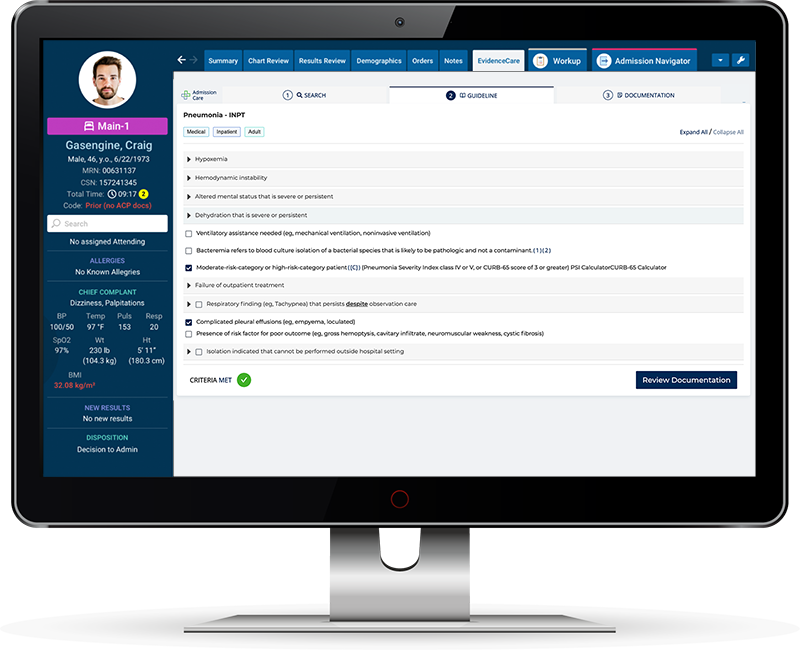
Today, EvidenceCare uses one of the types of hospital admission criteria, MCG criteria. Our AdmissionCare software is integrated into the physicians admission workflow in their EHR, so doctors can rely on a digital resource to evaluate a patient’s condition and automatically let doctors know whether a patient qualifies for admission or not. Interqual has created equally rigorous and useful guidelines for emergency departments and hospitals to make their own independent decisions about which of the two types of hospital admission criteria guidelines they are going to use in their emergency rooms to guide patient admission decisions.
There are several benefits to using evidence-based guidelines for hospital admissions decisions. First, it removes the guesswork for doctors who need to decide on the spot, whether patients should be admitted to the hospital as ‘inpatient’ or to ‘observation’ level of care. When they can refer to a set of criteria, doctors can simply compare patient’s medical condition to a well-respected, trusted resource and have an answer in seconds on the correct patient status, along with specific documentation to support that level of care.
For physicians, hospital administrators and utilization review teams, admission criteria software also ensures correct medical necessity documentation for insurance – saving a lot of time and effort during the patient’s stay by preventing back and forth with UR teams and peer to peer reviews with insurance companies. Nobody likes to have their decision questioned, but you must rely on your documentation to defend yourself.
Examples of Inpatient vs Observation Status
It can be hard to understand what constitutes the conditions required for inpatient hospital admission versus an observation stay. Hearing a few real-life examples of inpatient vs. observation status stories can help you better understand under what conditions doctors would admit patients—and under what circumstances doctors would place a patient in observation.
One health condition to consider when it comes to hospital admission criteria is heart failure. Heart failure is an acute health condition, but it does not always qualify a patient for inpatient admission. When a patient experiences ‘heart failure’, they can be placed in observation status to see if the treatment plan will alleviate the patient’s symptoms in a short period of time and be discharged home safely. However, if a patient does not improve with the treatment plan and requires a longer more intense treatment plan, inpatient care would be more appropriate.
For example, if the patient has pulmonary edema, requires nasal cannula to increase oxygen saturation, and Lasix, this patient could be treated in observation versus a more acutely ill patient who required more invasive ventilation and specialized acute care treatment.
It will all come down to what is documented as the acuity of the patient and treatment needed to stabilize the patient.
By having a tool like AdmissionCare to assist with these determinations, physicians and admitting practitioners can make quick, precise decisions about the best course of care for their patients.
Hospital Admission Software
One way to make the process of hospital admissions more accurate, faster, and less stressful is by using admission criteria software. A bed status decision software like AdmissionCare reduces the burden of administrative work on doctors and allows them to do what they do best—care for patients’ health.
Giving doctors a medical necessity documentation software like AdmissionCare empowers physicians at the point of care, and its ease of use reduces the amount of work required for everyone involved—no heavy tech training necessary. If your hospital or health system decides to start using AdmissionCare, you can benefit from perks like:
-
- Speeding up the patient handoff process
- Determining bed status without rigorous training
- Reducing administrative workload for physicians
- UR/Insurance will not interrupt physicians
- Satisfaction that your status is correct, you have documentation to support it, and you ultimately made the best decision
To learn more about the best inpatient vs outpatient software available watch this video about AdmissionCare and how it can improve your hospital admission process. You can also schedule a demo if you’d like to see what it’d be like to use AdmissionCare with your EHR.