Denial Management Workflow
Hospitals often struggle to get paid for the services they provide patients. One reason is that insurance companies can make it difficult to file all the necessary paperwork to have a claim accepted and covered, and hospitals often receive claim denials, creating bottlenecks in their revenue stream.
Even with all the denial management workflow improvements and companies focused on claim denials, recent research still shows hospitals have a denial management problem.
Denials in healthcare are common for claims from emergency departments (EDs), not only because the claims they file are often for pricey procedures that require costly reimbursements, but also because the in-depth administrative requirements can slip through the cracks or be left to physicians who already have vital responsibilities in patient care.
Because of how common denials are, hospitals have had to come up with elaborate, well-established ways to handle denials in medical billing.
Most medical practices or hospitals have a denial management workflow involving a backend team after patients have received care and been discharged. Staff dedicated to denial management often work in the billing or revenue cycle department and must discover the cause of the denial and appeal it.
Using a computer or web-based program for the management of admissions and bed status decisions can help make these situations easier — and even avoid them in the first place.
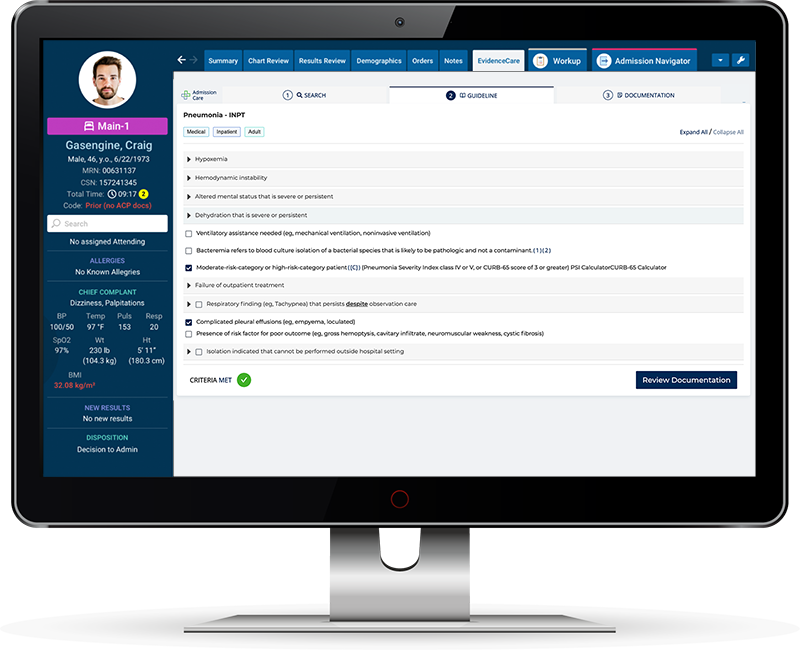
Denial management software tools make decisions more precise and accurate for physicians. The best kinds of denial management software empower accurate documentation on the frontend of the process and work with all kinds of EHRs (electronic health records), so physicians can access them while looking at a patient’s record. This eliminates the need to flip back and forth between programs and documents, have backend staff interrupt physicians for past claims, and minimizes the cognitive energy required for any task other than treating sick patients.
When hospitals use frontend denial management software, they can file the right documentation the first time, ensure patients are covered for the treatments they’ll receive, and avoid denial management entirely.
Here’s what you should know about denial management workflows and how digital tools can transform your hospital revenue stream into one that flows easily and without hiccups.
Denial Management Process
Hospitals rely on payments from insurance companies for a significant portion of their revenue. When medical decisions and administrative processes operate successfully, insurance companies pay the claims submitted to them, and hospitals receive payments for the treatments they provided and materials they used for care.
However, an extremely common block that hospitals often have to deal with in their revenue stream — which can actually make or break the ability of a hospital to function — is claim denials.
Insurance companies may issue claim denials when they receive requests to reimburse a hospital for the care provided to an insured patient. When a claim denial is issued, that denial goes to those in charge of *denial management* at the hospital.
What is denial management?
Denial management is the process of dealing with insurance company denials at a hospital. Every organization has a different claims denial management process. Denial management in healthcare can be handled by hospital administrators, billing departments, or professionals solely dedicated to managing denied claims in healthcare.
Denial management is NOT the same as insurance claim rejection. The difference between rejection and denial in medical billing is that a rejection happens in a hospital’s clearing house and happens before the claim ever reaches an insurance company. A rejection usually means there is a clerical error that needs to be remedied to allow an insurance company to even accept a claim. When a claim denial happens, an insurance company has processed the claim, and they have decided they will not cover it.
Claim denials can happen for a slew of reasons, e.g., the right paperwork isn’t completed and filed or a doctor hasn’t proven that a treatment decision was medically necessary. If, through a denial management process, a hospital is able to provide the right paperwork or show that the treatment was necessary, an insurance company can decide to reverse their denial and cover the claim.
Medical Necessity Denials
While insurance companies do issue denials for errors or omissions, there are also times that insurers issue medical necessity denials. These denials happen when insurance companies look at claims and determine that the procedures done for patients were not medically necessary. To cover healthcare costs, many insurance companies insist that the course of treatment provided must have been absolutely necessary.
If an insurance company believes a hospital provided treatment to a patient that was not necessary for them to live or heal, their response to the hospital will be: claim denied as not medically necessary.
There are many reasons that medical necessity denials happen. One of these reasons is a lack of medical knowledge on the part of the insurance company or unclear documentation on the part of the hospital’s physician. Hospital administrators can issue further documentation explaining the course of treatment. Insurers may also issue a “claimed denied as not medically necessary” if a medical team actually does make an error.
All healthcare providers are ethically obligated to treat their patients with their well-being in mind. However, the pressure of working with critically ill patients can make it difficult for physicians, nurses, and other hospital staff to avoid errors 100% of the time. This is especially true when doctors are saddled with more tasks than just providing medical care — like administrative work. The more matters a doctor has to focus on, the more likely they are to accidentally let one area slip. And often it isn’t an error, but a misunderstanding of what was required for medical treatment between the insurance physician and the hospital physician.
Software programs that help manage bed status decisions and claim denials are an effective way to reduce the amount of mental energy and effort a doctor must use while treating a patient. That way, they can focus solely on medical care and make sure they make decisions that include only the most medically necessary treatments with the documentation to support the decision.
Top 10 Denials In Medical Billing
It may be surprising to know that insurance companies regularly issue hard denials in medical billing. While patients are not privy to medical billing denial codes and reasons, these denials end up on the desk of hospital administrators and revenue cycle departments who then have to chase down payments for care, materials, and procedures previously provided (and completed) to patients.
Insurance companies deny claims for many reasons, and reading through a list of denials in medical billing helps understand why. Even the most common denial codes might surprise you, even if you work in healthcare.
Here are the top 10 denials in medical billing that often leave hospital administrators frustrated, with extra work to do, and hurting for revenue:
-
- Registration/eligibility
- Missing or invalid claim data
- Authorization/pre-certification
- Service not covered
- Medical documentation requested
- Medical Necessity
- Untimely filing
- Medical Coding
- Provider eligibility
- Avoidable care
While there are many types of denials that hospitals receive, there is actually one best way to handle those denials: stop them before they ever occur. Effective claims denial management includes collecting all necessary information from patients and clinicians from the get-go and being certain all necessary paperwork and documentation is completed for every patient who receives care.
To ensure this level of precision specifically in an emergency department, it helps to equip physicians, nurses, and staff with tools to help them get the admissions process and bed status decisions right. One of the best tools available today for smoothing out workflow and increasing hospital revenue is denial management software.
Denial Management Software
While there are several tools for hospital administrators to fight denials on the backend, one of the best tools is denial management software used during admissions. This can stop denials before they can even happen.
EvidenceCare created EHR denial management software called AdmissionCare that helps doctors make appropriate bed status decisions and get the documentation needed for hospitals to avoid medical necessity denials for patients at the time of admission.
AdmissionCare being integrated into the EHR also helps admitting physicians and inpatient teams by:
-
- Improving clinical workflow so the ED operates more smoothly and patients are more satisfied with their experience at a hospital
- Reducing medical necessity denials and documentation queries, which create headaches for billing departments and clinicians retroactively
- Helping with timely claim filing
- Accelerating handoffs between emergency physicians and inpatient teams
- Removing interruptions from utilization review and physician advisors
- Creating a clinically-driven revenue cycle
- Increasing revenue for hospitals by eliminating the need to spend resources on appeals and by decreasing the number of claim denials
By using EMR denial management software, like EvidenceCare’s software, AdmissionCare, you can ensure you get medical necessity documentation right in the EHR/EMR, and make life easier for doctors in the emergency department.
With medical necessity software for doctors, you can not only reduce medical necessity denials but also help increase physician job satisfaction and reduce physician turnover in emergency departments. Doctors can focus more on doing their job — caring for patients’ health — and less on handling administrative tasks and clunky tech programs that require extra energy and effort.
With AdmissionCare, you can ensure your hospital decreases medical necessity denials further down in the process after the patients leave the hospital, and make everyone touched by the hospital admissions and insurance process happier and more satisfied in the long run.
Schedule a demo of AdmissionCare today!