Medical Necessity Documentation Requirements
Many doctors, nurses, and healthcare workers are overworked, overstimulated, and drowning in administrative process. Processes like determining bed status and medical necessity are significant features of administration work that doctors have to deal with daily.
The administrative burden on doctors and other clinicians is becoming overwhelming, with many doctors stretched too thin to have any sort of optimal clinical workflow. There is a clear need for an operational change in administrative work and medical necessity documentation requirements in healthcare settings.
While there is no single process or medical documentation guideline for documenting medical necessity, as each patient is unique, some medical record documentation requirements should be implemented to keep medical documentation as streamlined as possible.
One example of standardization and guidelines for patient insured by Medicare and Medicaid is CMS physician documentation requirements, as they detail every document a healthcare facility needs to use to complete the medical necessity documentation requirements.
Several areas of medical documentation need to be completed and filled out correctly by doctors. One of the most critical pieces of information is the evaluation and management of CPT codes that healthcare professionals use to represent the service they provide to a patient. They include office and hospital visits and are mainly used by consultants, emergency room physicians who are short on time, and primary care doctors.
These are especially important as these codes show what work a doctor has completed and what work a healthcare facility can bill for.
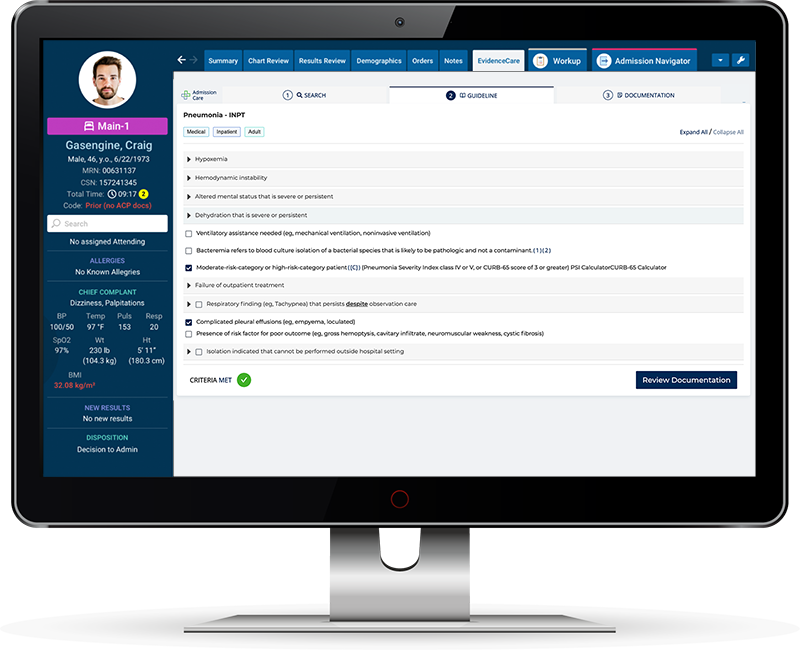
Implementing a software system like AdmissionCare could automate the necessary medical documentation that doctors have to generate and help with CPT codes. It would take the ever-increasing administration burden from physicians so they could focus more on patient care.
CMS Documentation Guidelines 2023
Most physicians and healthcare professionals follow the CMS documentation guidelines 2023 to ensure quality documentation is filled out and filed for patient records all the time.
CMS documentation guidelines 2023 are split up into three main sections:
-
- CMS medical record documentation guidelines 2023
- CMS timely documentation guidelines
- CMS Evaluation and management guidelines 2023
CMS Medical Record Documentation Guidelines 2023
Here are some of the main CMS medical record guidelines for 2023:
-
- All medical records should be legible and clear.
- All records should be appropriately signed; handwritten and electronic signatures may be used.
- Services that are time-based must include the duration of the service. This consists of the time allocated to medical-decision making.
- Any documentation should be signed as soon as possible after medical treatment has been allocated.
- Medical records cannot be altered.
- Each medical record must be specific to the patient and provided with enough information so a reviewer is confident that the correct medical treatment was administered.
- If any anomalies occur on the medical record, a doctor can add a note at the end with an explanation.
CMS’s timely completion of medical records involves doctors completing medical records during an encounter with a patient or directly after. While they do not provide a specific timeframe, best practice determined that 24-48 hours is reasonable. Medicare documentation requirements state that all documentation must be completed before submission.
What are Evaluation and Management Services?
Evaluation and management services are when a doctor or healthcare worker diagnoses and treats a patient with a specific illness or injury. Most doctors provide this service to their patients. Appropriate documentation and coding of evaluation and management services are critical as they capture the medical treatment provided.
CMS Evaluation and Management Guidelines 2023
The CMS documentation guidelines for evaluation and management services have changed a number of their procedures this year. There are seven components to E/M documentation:
-
- History
- Examination
- Medical decisions
- Counseling
- Co-ordination of Care
- Nature of Presenting Problem
- Time
If a doctor simultaneously works their way through these steps, then the documentation should be accurate and sufficient.
How to Document Medical Necessity
Medical necessity is intended to determine if a specific treatment or procedure was necessary based on a patient’s medical condition and best practices. It can often be a battleground between providers at hospitals and insurers as to what is medically necessary.
How to Document Medical Necessity?
When a patient comes into a healthcare facility and needs treatment for an ailment, an evaluation is completed to determine their care level.
Firstly, it needs to be decided if they will need hospitalization. To determine this, the patient needs to meet the criteria for hospital admission or medical necessity, which occur as:
-
- The severity of symptoms exhibited by the patient
- The probability of the patient getting worse without hospitalization
- The need and availability of a doctor to complete a diagnosis
It is up to the doctors to determine if there is medical necessity for inpatient admission. The inpatient medical necessity would include that the patient’s condition would worsen if not in a medical facility, and the patient’s medical record or EHR and supporting documentation should reflect that.
Patients undergoing short hospital stays may be treated similarly to inpatients but are classified as outpatients on medical documentation. Depending on the patient’s condition, they will be under either inpatient medical necessity or observation medical necessity. Outpatient medical necessity is patients under observational care and is described as having a short-term treatment that the doctors will assess before either being discharged or requiring further treatment as an inpatient.
Hospital admission is a notoriously complex decision-making process. Still, if the doctor decides that the patient is to become an inpatient, they must complete a hospital inpatient admission order. Hospital inpatient admission is deemed necessary when the patient stays across two midnights, named the two-midnight rule by CMS; anything under two nights is considered an outpatient.
By determining the patient’s status, medical necessity can be documented easily on an EHR or an EMR, as the diagnosis and treatment of the patient will determine what documents need to be used during their medical treatment.
Medical Record Documentation Best Practices
To ensure every patient’s medical records are completed and are at the best standard, here are some of the medical record documentation best practices:
-
- Review a patient’s medical necessity for hospital admission; whether they have just arrived or are in the outpatient section, they should be reviewed regularly to assess their condition. The medical necessity documentation should include the specific reason for the visit and the rationale for keeping the patient in the facility. Evidence-based guidelines such as MCG Guidelines or Interqual Guidelines are excellent for making the best medical necessity documentation.
- Convey the entire medical process; medical documentation should tell the story of the patient’s journey through the healthcare facility. It should include the patient’s past health information, if it is relevant, and an evaluation of the treatment method used. Do not miss critical details.
- A patient’s treatment plan can be reviewed by another if the primary treatment is ineffective. A utilization review process is a technique that should be used to determine the medical necessity of the procedures and treatment for a specific patient. The UR team is excellent at determining if a patient needs an alternative treatment process or needs better documentation.
- Make sure records are clear, accurate, and legible.
- Move to digital records, as it will streamline the documentation process. Digital medical documentation examples include an EMR or EHR.
- If any information is added at a later date, sign and date it so if an impartial person was reading it, they would understand the sequence of events.
- If inaccurate information is discovered, take immediate action.
- Adhere to official documentation retention periods, which will be detailed in CMS medical record documentation guidelines 2023.
- When it comes to operative reports, they should have the operation that was performed, the time and date of the operation, the team performing the procedure, the preparation of the patients, and then the full details of the operation process, see CMS operative report documentation guideline for a more comprehensive guide.
Medical Necessity Software
Determining medical necessity is something that doctors have to do several times a day for many different patients with a range of ailments. Physicians weren’t trained on the proper criteria determined by organization such as CMS, MCG, and Interqual that insurance companies use for medical necessity. Keeping up to date on these criteria is a labor-some and inefficient use of their clinical expertise, often focused on by clinical utilization management staff. Implementing a software platform such as AdmissionCare can relieve this burden.
AdmissionCare is a medical necessity documentation software. It helps by giving admitting physicians and hospitalists the guidelines needed for a patient’s bed status and documenting them correctly in the EHR. This will save any downstream issues for UR and insurance and reduce denials.
There are constant changes in the documentation needed to admit a patient into a hospital. This year, the CMS H&P documentation requirements 2023 and the CMS operative report documentation guidelines have been revised. But AdmissionCare can help with that. It contains software for documenting hospital admissions to make it more efficient and streamlined. It has the ability to automate inpatient vs. observation documentation so that it can be easily changed if a patient switches status.
When a patient becomes an inpatient, there is specific inpatient documentation software to add all the necessary documentation, which makes it easier for one doctor to hand over to the next doctor. It reduces documentation queries and medical necessity denials.
Overall, it is a medical necessity software that can increase revenue through appropriate bed status decisions and streamlining the medical documentation process throughout departments, empowering doctors and improving the overall revenue of the hospital.
Contact EvidenceCare and start your healthcare facility’s journey to more streamlined medical documentation with AdmissionCare.
Schedule a customized demo today.