Reducing Observation Status
Observation status in the emergency department is a patient or “bed” status hospitals use to monitor patients who aren’t ready for discharge but don’t meet the criteria required for a full inpatient admission. Reducing observation status, therefore, refers to minimizing the time patients spend under this particular classification. It’s an important part of both the patient experience and a hospital’s revenue and billing abilities, influenced by guidelines provided by the Centers for Medicare and Medicaid Services (CMS), evidence-based criteria providers, and other insurance companies.
Hospital observation status enables healthcare institutions to evaluate a patient’s condition over a short period, typically ranging from 24 to 48 hours. This strategy, while beneficial in certain scenarios, has implications that impact a patient’s stay in the emergency room or other hospital departments. As patients under observation are not officially admitted, many services they receive during their stay may not be covered by their insurance. Under observation in hospital means an interim phase where healthcare practitioners can make a definitive decision about whether a patient should be admitted for further treatment or is safe for discharge.
Unfortunately, for many doctors and hospitals, observation status has been treated as simply a “holding area” for gray cases or those they believe will be less than 48 hours without as much thought given to medical necessity and evidence-based guidelines. Appropriately reducing observation status can lessen a patient’s financial and psychological burden and improve the efficiency of hospital processes.
So why do hospitals use observation status?
Hospitals often resort to the use of observation status to comply with CMS guidelines. The tough scrutiny of “medically necessary” admissions by Medicare has led hospitals to admit patients under observation status to avoid potential penalties. The reimbursement rules dictated by CMS have a significant influence on the hospital’s decision on whether a patient should be designated under observation status or fully admitted.
While this process can seem bewildering, understanding the reasons why hospitals use observation status is a helpful first step in communicating with healthcare providers on how to make an informed decision about a patient’s status.
Because of all this, reducing observation status has become a prominent discussion in healthcare.
The Role of CMS in Observation Status
To better grasp the intricacies of bed statuses, it’s essential to understand the role of insurance. This complex system, intertwined with rules and guidelines established by the Centers for Medicare and Medicaid Services (CMS), has a significant influence on situations like:
-
- The switch from observation to inpatient status
- The application of the CMS Two-Midnight Rule
- The definitions and differences between the SNF 3-day rule (sometimes referred to as the Medicare 72-hour observation rule)
Insurance providers play a pivotal role in these processes. For instance, the choice to shift a patient from observation to inpatient status should be based on patient severity or worsening condition but can often hinge on insurance rules and stipulations. Typically, in cases where a patient does not meet certain criteria for an inpatient stay, the patient would be placed in observation status. The transition to inpatient impacts the way insurance providers deliver coverage, often resulting in incremental costs to the patient.
Adding another layer to the complexity are guidelines such as the CMS Two-Midnight Rule. This Medicare policy states that generally, if an admitting physician expects a patient stay in the hospital to cross two midnights, it should be classified as inpatient, whereas those not expected to cross two midnights are supposed to be dealt with as outpatient or under observation status.
This general guideline has been incorrectly used as an absolute rule, even though there are exceptions to classifying patients as inpatient even when the hospital stay may be less than 48 hours. And while it’s a helpful guideline, some insurance companies have even suggested a 72-hour rule before inpatient admission.
Read more about exceptions to the two-midnight rule here.
The key is having the medical necessity documentation to support the patient status. Using evidence-based criteria is one helpful way to do that and avoids the gray area of time-based bed status decisions.
Lastly, Medicare has in place a Skilled Nursing Facility (SNF) 72-hour rule, or 3-day rule, stipulating that a patient must be under hospital care for at least three days before coverage for a subsequent SNF is granted. But here’s the catch: time spent under observation status often does not count toward meeting this requirement, potentially affecting Medicare coverage.
Guidelines and Limitations
CMS has very specific guidelines on how long a patient can be in observation status. According to these rules, the duration for a patient in this state should not exceed 48 hours, except in exceptional cases. You might ask, “Why would such a time limit matter?” The answer lies in the difference between hospital observation and inpatient admission status. Although seemingly trivial, the distinction can impact the level of reimbursement a hospital receives and how a patient is billed.
While hospitalizations under observation status are billed under Medicare’s Part B, admissions qualify for Part A, which is typically more comprehensive. This restriction can often lead to situations where patients who need extensive observation might find themselves on the unfavorable side of CMS observation to inpatient guidelines. These policies stipulate that a formal admission can only occur if a physician expects a patient’s treatment to span at least two midnights. This definition leads to gray areas that can cause confusion and possibly financial distress for patients.
In essence, CMS guidelines for observation status shape a patient’s healthcare experience in significant ways. The more someone understands these measures, the more they can navigate the healthcare system.
Hospital Procedures and Costs
Understanding cost breakdowns in healthcare can be quite difficult, especially when it comes to inpatient and observation status. Over recent decades, hospitals have used observation status more often, a decision driven by factors such as:
-
- Medicare payment models
- Risk management
- Service quality
Let’s recap these two statuses for clarity:
-
- Observation status refers to when a doctor needs additional time to determine if a patient should be formally admitted to the hospital as an inpatient. The length of a patient’s observation stay in a hospital can vary, lasting anywhere from a few hours to several days, depending on the medical circumstances. Commonly maintained for less than 24 hours, it can sometimes go up to 48 hours.
- In contrast, inpatient status is assigned when a doctor expects a patient’s care to extend beyond two midnights.
While these two statuses may seem very similar to a patient, their definitions have a substantial impact on how services are billed, and this is where observation status billing comes into play.
As previously mentioned, observation status is generally less expensive than inpatient status because it is billed under Medicare Part B (outpatient services), whereas inpatient services are billed under Medicare Part A.
The distinction between outpatient in a bed vs observation can be quite perplexing, too:
-
- An outpatient in a bed, unlike an observation patient, never got past the ER. The difference also extends to the billing side, with insurers using different models for reimbursement.
- An observation patient, despite having a designated bed in the hospital, is still categorized as an outpatient, resulting in varying co-pays, deductibles, and, ultimately, out-of-pocket costs.
Outpatient observation status further complicates things. Under Medicare, hospital stays under 24 hours are classified as an outpatient observatory; anything past this boundary is inpatient service. However, problems can occur when the decision to assign an outpatient observation status is perceived as a business strategy, particularly, to avoid penalties from CMS for high readmission rates of inpatients. This can lead to more scrutiny and penalties during CERT (comprehensive error rate testing) audits.
Reducing the unnecessary inclination towards choosing inpatient or observation status based on a business or financial incentive and instead aligning it with actual medical necessity can significantly improve the downstream effects of admission decisions.
Transitioning Observation to Inpatient Status
When patients are admitted to a hospital, they’re often classified under two categories: inpatient or observation. This categorization determines how both Medicare and the hospital will bill for services rendered during the patient’s stay. However, the process of transitioning observation to inpatient status can sometimes pose challenges by implicating the patient, the healthcare providers, and the insurance companies involved.
Observation status has come under scrutiny. This is primarily due to the cost and billing implications on the patients themselves. Again, that’s because patients under observation are considered outpatients and often pay higher out-of-pocket costs and different coverage from inpatient care. Medicare pays for observation under outpatient rates, generally at a lesser amount when compared to inpatient rates.
This leads us to a key topic of this article: how to facilitate the transition from observation to inpatient status. Changing patient status after discharge is, in general, seen as a red flag by regulators, and can lead to increased audits, penalties, and denied claims.
There are some extremely specific scenarios where a change is permissible, guided by complex and strict rules. Predominantly, an order from a competent physician that states that such a change is medically necessary is required. It is also beneficial to help patients understand this complexity, and this is where issuing a Medicare Outpatient Observation Notice (MOON) comes in.
Hospitals are required to provide a MOON to Medicare beneficiaries placed under observation status for more than 24 hours. The notice explains that they are outpatients receiving observation services, not inpatients, and highlights the financial implications of this status.
To conclude, transforming observation status to inpatient can be a regulatory minefield. However, it is certainly possible. Ultimately, patients should receive the care they need regardless of their status.
Automating Hospital Admission Criteria
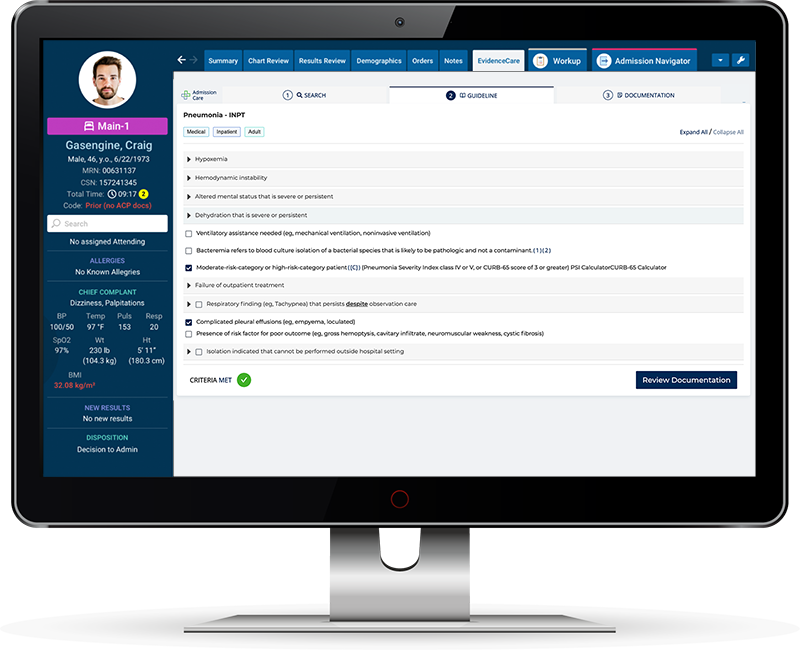
Because understanding the guidelines and limitations of observation status and inpatient status in hospitals can be quite complex, hospitals should equip doctors with hospital admission software, ensuring they easily understand the nature of observation and inpatient status and how guidelines like the CMS Two-Midnight Rule impact their decisions.
Because of innovative software like AdmissionCare, physicians can avoid the guesswork of choosing a patient status by automating admission criteria at the point of care in the EHR. This ensures admitting physicians have the medical necessity documentation to support their clinical decisions for inpatient admissions or observation status.
If you’re a hospital in search of a way to streamline admissions and avoid denial and audit issues, schedule a demo of AdmissionCare today!