Medical Necessity for Hospital Admission
Hospital admissions usually take place when a doctor identifies the need to manage a health condition or injury. Medical necessity for hospital admission indicates the patient’s condition may worsen if they do not get adequate care within a hospital setting and is usually a term used for the documentation surrounding the admission. Upon conducting a comprehensive patient examination, physicians determine the need for hospitalization and issue admission orders or not accordingly.
The decision to admit is often critical. Several factors are examined when a physician considers the requirement for an acute inpatient admission. The patient’s symptoms and signs are assessed alongside the potential course of treatment.
An important part of this evaluation is determining whether the patient’s acute condition requires immediate action. Simultaneously, the healthcare provider gauges the intensity of care services the patient might need.
Admissions follow established guidelines, and each hospital has policies for admission and discharge. So, when does inpatient admission start? A person becomes a patient when admitted and occupies a hospital bed for at least one night. Consider a scenario in which a patient has undergone certain procedures, and their doctor deems it necessary to admit the patient at 9 p.m.
In the above scenario, admission starts when a physician issues the orders and completes the medical necessity documentation. However, the patient might remain in the emergency or waiting room for some time as nurses and other staff prepare relevant documents. The team must also check bed availability before swinging into action.
Notably, hospital bed and accommodation billing commence on the admission date as indicated in the physician’s report. The medical provider qualifies a patient’s condition as medically necessary for hospital admission. Whether the need for hospitalization is for further observation or inpatient, physicians must state their reasons.
Hospital admission typically becomes medically necessary when a physician diagnoses a condition that can’t be treated on an outpatient basis. Furthermore, hospitalization becomes essential when the diagnosed condition demands ongoing and meticulous monitoring.
Inpatient Admission Criteria
Normally, patients are admitted to hospitals based on the severity of their illness, the necessity of medical treatment, the presence of chronic conditions, and the need for diagnostic procedures and monitoring. A doctor may determine that hospitalization is required following an outpatient’s medical examination. The doctor informs the patient of this decision and officially records the admission into the hospital’s electronic health record system.
Hospital admissions are systemic and require confirmation of bed status before anything else. Once sorted, the admitting personnel obtains a patient’s bio-data and the attending physician’s name. The hospital also assigns a patient identification number that helps track billing and medical records. The criteria for inpatient hospitalization has many factors to consider.
Hospitals rely on various types of hospital admission criteria to determine whether a patient should be classified as an inpatient or placed under observation status. Three commonly used sets of guidelines are the Milliman Care Guidelines (MCG), InterQual, and the Centers for Medicare and Medicaid Services (CMS) guidelines.
By following these observation or inpatient admission criteria, hospitals can ensure that patients receive the appropriate level of care based on their medical needs.
Understanding and implementing these guidelines are essential for hospitals to provide high-quality care, optimize resource utilization, and ensure compliance with reimbursement regulations.
While comparing hospital observation vs. admission, it’s important to also capture the medical necessity documentation in the EHR to stop denial issues at the source.
CMS Observation to Inpatient Guidelines
Let’s focus more on some key components of CMS guidelines. First, despite documentation criteria changing, the admitting physician reserves the decision to determine a patient’s status – the issue is more around the hospitals getting paid for that status. Generally, the CMS physician order requirements stipulate that patients should be admitted as an inpatient if their medical condition requires hospital care beyond two midnights.
Careful, accurate billing of inpatient hospital services is critical to ensure the hospital receives payment upon claim submission. CMS inpatient billing guidelines stipulate that healthcare providers only charge for services provided, including those of their physicians. On the other hand, the provider must submit a medical record summary, a discharge summary, and a physician’s order.
CMS guidelines for inpatient admission 2023 retain the same CPT codes for billing inpatient and observation care. Also, the Evaluation and Management (E/M) services title has been updated to Hospital Inpatient or Observation Care. Providers employed distinct codes for each of these in the past, but they are now consolidated into a single E/M code. There are detailed aspects of these guidelines, which providers meticulously put into action.
CMS sets these requirements and guidelines to standardize healthcare billing and improve quality. The oversight body plays the following roles:
Program Oversight
CMS’s oversight role is instrumental in ensuring that healthcare providers obtain reimbursement for costs billed under the Medicare and Medicaid programs. Failure to follow the facility observation guidelines may result in the rejection of claims or deregistration from the health coverage program.
Regulation
As a regulatory authority, CMS develops and implements rules that govern healthcare delivery. Through these regulations, the American public can access quality care. At the same time, patients are assured of safe treatment and access to specialized care at an affordable cost.
Payment for Medical Services
Payment policies under Medicare and Medicaid are also the prerogative of CMS. The federal body sets reimbursement rates and implements alternative healthcare payment models.
Hospital Admission Documentation Requirements
Hospital admission documentation requirements for medical necessity must meet the specificity rule. Healthcare providers should detail the signs and symptoms that necessitate admission. Also requiring documentation is the diagnosis, expected hospitalization length, and possible adverse outcome.
Here, a physician must carefully, and elaborately, detail the illness or injury and the risk emanating from treatment. The physician should indicate in the medical record documentation that the hospital stay involves eight hours but does not exceed 24 hours. Medical necessity guidelines also require documentation that proves the physician performed the stated services.
Furthermore, healthcare providers must follow the medical necessity criteria for documenting:
-
- Major and minor procedures
- Surgery performed, when applicable
- Tests performed on a patient
- Therapeutic services offered, if any
- Pharmacy prescriptions
- Patient’s observation status
By adhering to medical necessity requirements, hospitals support their decision to admit patients and are also part of the CMS regulations. Here’s how providers document medical necessity for inpatient care:
History of Present Illness
On the admission documentation, the hospital should briefly describe why the patient sought medical attention. It must also state the symptoms that led the physician to decide that an admission would suffice.
Past Medical History
A patient’s history offers insight into their current status and helps doctors prepare a treatment plan. Hospitals must document this as part of the medical necessity requirements. The details documented include allergies, previous surgery, and pre-existing conditions.
Laboratory Test Results
Before a patient gets hospitalized, they are first attended to as an outpatient. A doctor orders laboratory tests to confirm the ailment or its cause. By extension, healthcare providers must include the findings of these tests in the admission documentation.
Treatment Plan and Risk Assessment
The hospital, through its physicians, should follow the hospital admission criteria by stating the clinical judgment and admission rationale. In that rationale, the provider should also outline the planned treatment during hospitalization.
Medical Necessity Software
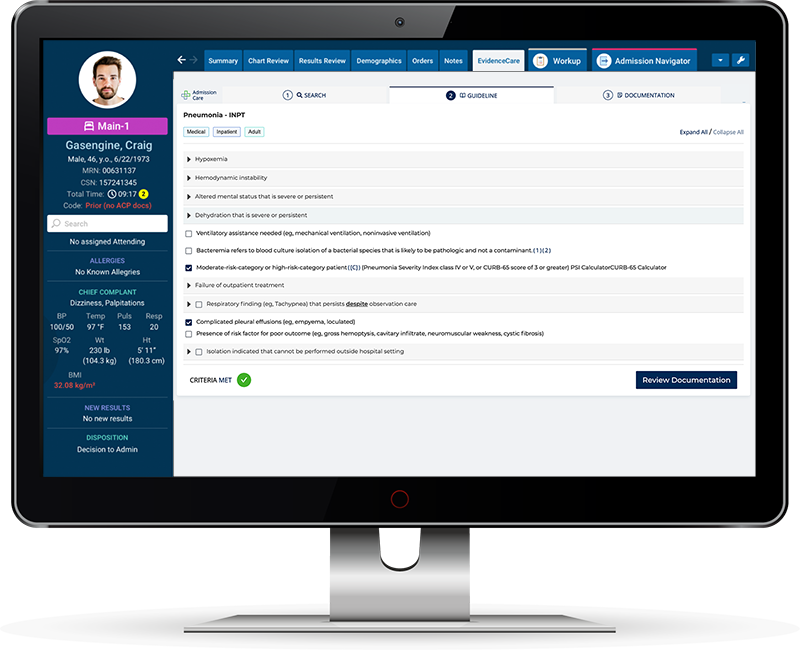
Hospital admission software like AdmissionCare can save a ton of time processing and documenting hospital admissions. The software also enhances data capture accuracy, ensures real-time access to inpatient vs observation criteria in the EHR, and prevents denials and missed revenue associated with inaccurate or poor documentation. It ensures hospitals meet the requirements for medical necessity admission.
Here are the benefits of hospital admission software:
Efficiency
Medical necessity software automates the process, ensuring providers fully control the admission process and subsequent documentation. Even more beneficial is that no extensive, time-consuming paperwork or manual data entry is involved. The result is an efficient admission process.
Regulatory Compliance
By utilizing admission criteria software, healthcare providers remain on the safe side of CMS and other regulatory compliance. The software streamlines compliance by providing all the requirements at the press of a button. Moreover, hospitals that implement medical necessity software lower the risk of penalties.
Data Access, Analysis, and Reports
Automated software enhances data access in real time. Hospitalists and admitting physicians can quickly find the information they need, prompting fast decisions. Furthermore, automated medical necessity in the EMR generates the required documentation automatically.
Short Turn-around Times
By automating admission criteria, hospitals process patients faster and more accurately, and patients have a better experience with timely, prompt care, especially for emergencies.
Cost Savings
Hospital software can be a big initial investment in time and resources, however, hospitals using AdmissionCare have seen incredible ROI by capturing revenue and reducing administrative burdens on their clinicians.
AdmissionCare takes care of medical necessity documentation requirements and integrates directly into the physician’s EHR workflow to guide them on bed status determination.
Schedule a customized demo of AdmissionCare today.