Changing Observation to Inpatient Status
Navigating the complexities of patient care status, especially the transition from observation to inpatient status is fundamental to operational efficiency and service quality in healthcare. The terms “observation” and “inpatient” are not just designations. The chosen status guides and shapes the diagnoses, interventions, and care trajectories that patients experience as well as the billing of both the patient and hospital.
This understanding is critical when considering changing a patient’s status from observation to inpatient status. It’s not just a clinical decision. It’s also an administrative and financial one. The switch can influence reimbursements, patient out-of-pocket costs, and coverage for post-hospital care. It also carries implications for the operational aspects of healthcare service.
For the uninitiated, observation status is when patients require additional monitoring after their initial examination or diagnostic tests in a hospital, typically lasting 24-48 hours. During this period, healthcare teams determine the need for further hospital admission or whether to discharge the patient with instructions for care at home.
Sometimes, the initial observation period requires an observation to inpatient status change. This transformation requires the doctor to substantiate the medical need for hospital admission by specifying the rationale for inpatient care, including the need for
-
- Comprehensive round-the-clock care
- Intravenous medications
- Advanced diagnostic tests
- Surgery
The transition from observation to inpatient coding becomes more complex on the administrative side. This coding includes a wealth of information — diagnoses, procedures, supplies, and services — that aligns with reimbursement for care provided. Accurate coding is critical.
Outpatient to inpatient status change is another critical change. As outpatients not formally admitted require escalating levels of care, they transition to inpatient status.
Similar to the change from observation to inpatient status, this requires explicit documentation and compliance with regulatory guidelines. Medical necessity remains the determinant for justifying this status change, again with financial and administrative consequences.
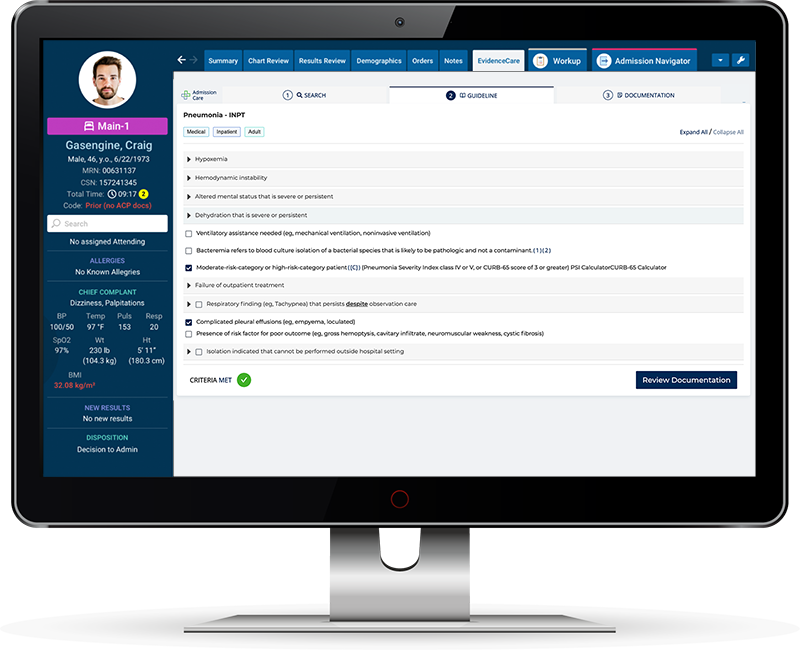
When considering how to avoid observation status, healthcare providers must make thorough assessments during the initial examination and continuously evaluate the need for inpatient care. Using admission criteria like MCG and Interqual combined with software like AdmissionCare can give admitting providers the medical necessity documentation needed to admit a patient. These steps minimize potential complications with insurance companies, utilization management staff, and ultimately, patients.
Initiating a status change from observation to inpatient is a process that requires a multidimensional approach. It calls for synchronization of clinical judgment, administrative rules and guidelines, and financial aspects. The goal remains to retain high-level patient care while keeping the workflow streamlined.
Rules and Guidelines
The healthcare system can be complex, with ever-evolving rules and guidelines. The transition from observation to inpatient status requires particular attention to align with insurance and CMS guidelines.
The Centers for Medicare and Medicaid Services (CMS) shapes policy and regulation to ensure quality healthcare provision. They have created specific CMS guidelines for observation status. These rules promote patient-centered care and streamline the work process for healthcare providers and administrators. Transitioning from observation to inpatient status is not arbitrary. It’s a process steeped in careful clinical scrutiny, administrative assessment, and due respect to the existing CMS guidelines.
Understanding observation status requires knowledge of inpatient vs. observation criteria.
Observation status generally refers to
-
- Short-term treatment and patient monitoring
- Diagnosing the patient
- Monitoring patient response to treatment
- Decide whether admission is advisable
Inpatient status generally refers to patients who
-
- Need two or more overnight stays.
- Require a critical level of medical attention.
- Need medical attention that’s not feasible as an outpatient.
We intentionally use the word “general” as there are exceptions to these benchmarks. For CMS observation to inpatient guidelines, physicians and other healthcare providers must comply with specific conditions for observation vs. inpatient admission decisions. Medicare observation to inpatient guidelines suggest the benchmark that an inpatient admission must exceed two midnights.
The “two-midnight rule,” as it’s called, is the threshold for transition from observation to inpatient status. Moreover, a careful understanding of observation to inpatient rules ensures efficient care delivery and avoids unwarranted insurance claim denials.
It’s critical to remember that the fiscal impacts of incorrect patient status classification can lead to hefty Medicare penalties. Remaining up-to-date and compliant with rules and guidelines for changing the observation status to inpatient is imperative for patient care and the healthcare providers’ reputation.
Coding and Billing
Many considerations come into the picture when dealing with healthcare coding and billing. Various conditional factors and ever-evolving regulations require careful navigation.
Aspects that warrant particular attention include changing status from observation to inpatient coding. Observation coding and inpatient coding represent two distinct billing entities in the healthcare system. These categories receive different treatment in terms of reimbursement rates and regulations.
A patient’s status transition from observation to inpatient may seem simple, but appropriate coding involves several significant steps and meticulous attention to detail.
One critical aspect to consider when transitioning from observation to inpatient coding is the adherence to specific “present on admission (POA) indicators.” These indicators play an essential role in identifying conditions present at the time of hospitalization. Accurate documentation of these indicators directly impacts the coding, funding, and planning processes. Therefore, accuracy in determining, documenting, and coding these indicators is paramount when transitioning from observation to inpatient status.
Additionally, using the right bill type is crucial. For example, when to use bill type 121 can be challenging without an in-depth understanding of specific healthcare billing regulations.
The billing and coding aspects of changing the observation to inpatient status involve accurate data collection, precise documentation, and a confident grasp of involved regulations. Healthcare providers and administrators must remain vigilant to ensure efficient transitions and rigorous compliance with all relevant protocols and guidelines. They can effectively maneuver through the complexities of coding and billing and improve patient care and organizational efficacy by paying careful attention to every detail, from patient admission indicators to the correct bill types.
Observation Status vs. Inpatient Admission
Navigating the intricacies of different hospital statuses can be complex, particularly concerning observation status vs. inpatient admission. These two classifications play a significant role in healthcare delivery. They influence patient care delivery and billing for services. Whether a patient qualifies for observation status or inpatient admission can significantly affect the guidelines physicians must follow and the financial implications for both patient and provider.
Hospital observation vs. admission (or inpatient) serves as two primary hospital classifications that dictate treatment procedures, cost, and Medicare coverage. While seemingly interchangeable, subtle differences between patient care, billing, and physician guidance make them distinct.
Observation status is typically applied when patients are not well enough to go home but are not sick enough to be admitted as an inpatient. It usually lasts less than 48 hours.
However, the question often raised is: How long can a patient be in observation status? According to Medicare rules, patients can be in observation status for up to three days, beyond which they should typically be admitted as inpatients or discharged.
Conversely, inpatient admission occurs when a patient’s condition necessitates more than 48 hours of hospitalization. This status often requires hospital resources beyond observation care. It also triggers a specific set of Medicare billing codes that allow the hospital to be paid more for the broader range of services provided.
Inpatient vs. observation Medicare coverage also presents significant differences. While both categories come under Medicare Part A, observation status may lead to less comprehensive coverage and additional out-of-pocket expenses for patients due to its short-term nature. On the other hand, inpatient admission usually offers more extensive coverage. Lastly, the decision between inpatient vs. observation status often lies with physicians. Factors such as expected duration of stay, severity of condition, and risk factors all play a role in this decision-making process.
It is crucial to navigate these parameters effectively to ensure accurate patient classification, appropriate care delivery, and fair billing practices, all of which contribute to superior patient outcomes. Understanding these complexities in healthcare status classifications cannot be underestimated.
Converting Inpatient Cases
The management and categorization of hospital admissions have often influenced funding, patient care quality, and health metrics’ accuracy. Converting inpatient cases to an observational status can significantly impact hospital operations, necessitating a thorough understanding of this critical process.
In an increasingly meticulous healthcare landscape, effectively switching from inpatient to observation status is pivotal. The reasons for such a transition vary. The patient’s health may have improved, requiring less intensive care. It might also be due to the patient’s condition not meeting the requisite parameters for inpatient care in the first place.
When converting inpatient cases, accurate and timely execution is crucial to avoid administrative confusion and patient dissatisfaction. However, hospitals may face challenges in determining when and how to transition, hence the need for sophisticated decision-support tools like admission criteria software.
This sophisticated technology helps healthcare providers make informed decisions about a patient’s status at the point of care with the correct documentation to justify their decision.
But changing inpatient to observation after discharge presents additional complexities. Strictly speaking, the patient’s status at the moment of discharge should remain unchanged, yet specific circumstances may necessitate a post-discharge adjustment.
Nuanced circumstances may present opportunities for quality improvement and enhanced profitability, highlighting the importance of broader discussions and targeted strategies to navigate these multifaceted patient care pathways. Prudent decision-making is paramount when bridging the gaps in patient care and hospital administrative processes. By understanding these intricate details of patient case conversions, healthcare providers can maximize their potential for operations optimization and overall improvement in patient care.
Overall, this is why EvidenceCare created AdmissionCare – to automate admission criteria for admitting physicians in the EHR, so that doctors get it right at the source, and hospitals have the documentation needed to get reimbursed appropriately.
Schedule a customized demo of AdmissionCare to learn more!