Utilization Management Software for Hospital Admissions
The growth of healthcare information technology in the past decade has yielded an impressive array of tools and solutions designed to optimize healthcare delivery, streamline workflows, and improve patient outcomes. One category that has been central to this growth is utilization management software for hospital admissions.
These sophisticated systems seamlessly handle the admission process while determining the necessity, appropriateness, and efficiency of healthcare services, equipment, and facilities. Healthcare utilization management companies have emerged as critical players by offering solutions to improve patient care while reducing operational expenses.
This type of software enables hospitals to
-
- Review and approve necessary treatments
- Avoid unnecessary hospital admissions
- Ensure appropriate patient placement
- Capture medical necessity documentation
- Facilitate efficient resource allocation and cost savings
- Improve service quality
- Ensure financial sustainability
Utilization review software, a significant component of utilization management, is instrumental in curbing unnecessary spending in healthcare. It helps in the healthcare provision audit process, ensuring that only necessary, quality care is provided. This software utilizes comprehensive schemes to evaluate medical necessity, appropriateness, and efficiency of healthcare services. Product-specificity stands as an essential factor when considering these technological resources.
Hospital admission review software, for instance, is custom-built to prioritize and manage patient admission procedures, enhancing efficiency and patient satisfaction throughout the admission process. This specialty software makes admission workflows smoother, reducing administrative tasks, and eliminating redundancies that may slow the process. However, identifying the best utilization management software (UM) can be challenging.
The ideal UM software should:
-
- Be capable of integrating seamlessly with existing EHR systems
- Offer flexibility for customization in the clinicians’ workflow
- Include a user-friendly interface
- Provide robust data security
- Offer real-time capabilities to help make informed decisions
Healthcare providers entrust a vital task to top vendors for utilization management software. These vendors provide the software plus implementation, maintenance, and updates, ensuring it aligns perfectly with providers’ demands. UM software for hospitals has significantly evolved, catering to needs ranging from inpatient utilization review to outpatient case management and protocols.
Inpatient utilization review software, specifically, is rapidly gaining significance in hospitals. These digital solutions efficiently manage and evaluate the medical necessity, appropriateness, and effectiveness of healthcare services provided to inpatients. Through these systems, healthcare providers are empowered with data-driven insights, facilitating strategic decision-making related to patient care.
Healthcare utilization management software has become central to efficient service delivery, offering solutions from admission to discharge. With the power of deep analytics and automation, these software systems are revolutionizing healthcare management, delivering better patient care, enhancing operational efficiency, and, in the long run, creating a sustainable healthcare environment.
Improve Efficiency and Accuracy in the Admissions Process
The healthcare industry has recognized the need to upgrade and streamline operations, making them more efficient and accurate. A core emphasis is the admissions process, a domain with a significant impact on the patient’s experience and the hospital’s operational workflow.
The right utilization management software can help streamline the hospital admission process. This innovation leverages software to manage and optimize patient admission procedures, ensure that patients receive the appropriate level of care, document that care correctly, and reduce the number of incorrect inpatient admissions or observation status placements, thus increasing overall operational efficiency.
By integrating patient status criteria – like MCG or Interqual – with patient data, this software determines the optimal level of care required, minimizing the likelihood of unnecessary admissions. This precise approach means time and resource savings for hospitals, ensuring that medical attention isn’t diverted from patients requiring hospitalization. It also has a significant impact on a hospital’s revenue and reimbursement rates.
Hospitals can implement concurrent review software for hospitals to refine the quality and precision of patient care approvals. In addition, maintaining a consistent line of communication with payers is fundamentally essential. Transparency and clarity can improve communication with payers and alleviate the administrative workload and financial uncertainties resulting from unapproved care or disputes related to payment and coverage. Utilization management software enhances the efficiency of the communication process and makes it less complex by effectively tracking and managing key information.
Adopting utilization management software along with care management software is an effective strategy to improve patient care. While care management software focuses primarily on coordinating patient care, integration with utilization management software can enable a comprehensive, patient-centric approach to healthcare delivery. This strategic partnership significantly improves the admissions process, helping hospitals balance the objectives of quality patient care with sustained operational efficiency.
One of the most significant advantages of this innovative software is that it combs through and analyzes vast amounts of patient data, providing insightful inputs that contribute to delivering patient-targeted care. These insights are invaluable, given their potential to foresee and promptly respond to healthcare needs.
To improve efficiency and accuracy in the admissions process, the role of utilization management software, particularly when paired with care management software, is paramount. Just a few benefits of this technological integration include:
-
- Assisting in communication with payers
- Conducting concurrent reviews
- Reducing unnecessary admissions
- Ensuring patients receive appropriate care
With the rapid progress in technology and healthcare, the expanding role of such innovative solutions will shape hospital patient admissions.
Hospital Admission Criteria
Hospital admission criteria represent a critical aspect of the admissions process and subsequent utilization reviews. These guidelines help determine the appropriate level of patient care while balancing the need for thorough documentation. Hospital admission guidelines standardize the decision-making process, ensuring more predictable reimbursement rates for hospitals and appropriate care for patients.
Quality patient care revolves around decisions like these, whether inpatient vs. observation status or an outpatient basis. InterQual and Milliman Care Guidelines (MCG), for instance, are robust utilization management guidelines that play a fundamental role in executing these criteria.
What is InterQual used for? InterQual determines the need, appropriateness, and duration of admissions. InterQual criteria help decide whether a patient’s condition meets the requirements for inpatient care. It helps ensure patients receive the right level of care at the right time. InterQual criteria for inpatient admission ensures the highest level of scrutiny in patient care.
Similarly, the Milliman Care Guidelines, also known as MCG, provide a comprehensive assessment of a patient’s needs, providing a consistent, evidence-based approach to care. Guidelines and tools like MCG and InterQual offer a reliable, standardized mechanism for making critical care decisions. These evidence-based companies can also reduce healthcare costs through improved efficiency and consistency in patient care.
While there may be slight differences between MCG and InterQual content, overall there is high concordance between them in regards to what patients they classify into INPT and OBS status. Providers and health systems are best equipped when using one of these tools as opposed to trying to do this on their own with nothing to reference.
It also ensures health systems have documentation defense against payers, especially with the Medicare 2 Midnight and Medicare Advantage rules. It all comes down to physician’s making appropriate bed status determinations and having robust documentation of medical necessity.
While new CMS rules have stated they don’t advocate for specific criteria (from MCG or InterQual), they do put the onus on the physicians to have proper documentation of medical necessity in terms of a patients expectation of care resources that will be needed during that hospitalization.
Best Utilization Management Software for Hospital Admissions
Healthcare technology offers many innovative solutions designed to streamline admission processes, improve patient outcomes, and optimize operational efficiency. Among the offerings, you’ll find the best utilization management software for hospital admissions that has revolutionized hospitals’ approach to ensuring positive outcomes.
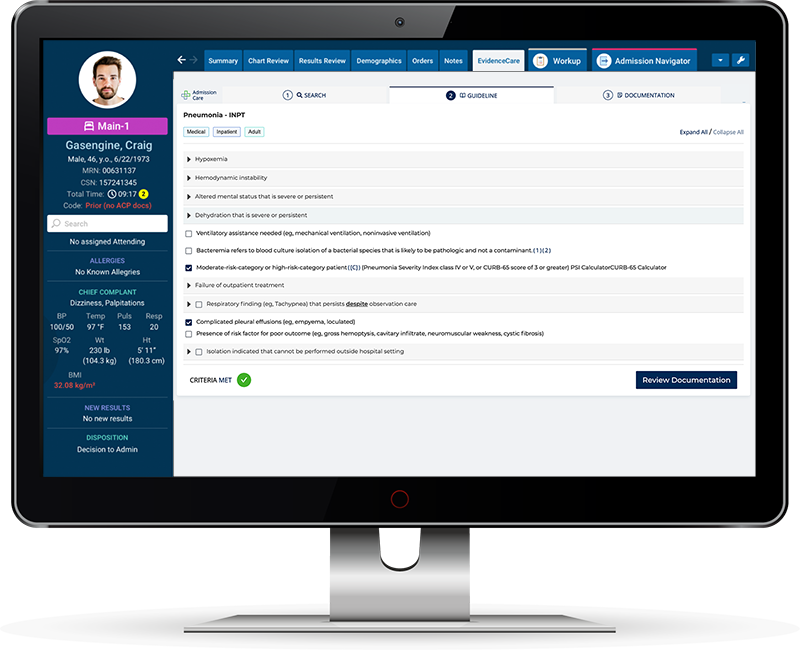
The best utilization management software optimizes the admission process by equipping admitting physicians with the criteria and documentation needed to make informed patient status decisions at the point of care.
That’s why EvidenceCare’s AdmissionCare product focuses on providing physicians with the criteria and documentation needed to help support their clinical decisions in their EHR workflow.
The many stringent requirements, regulatory compliances, and insurance criteria often make the hospital admission process a complex labyrinth to navigate. With that in mind, this utilization management software has been designed to simplify and streamline this intricate process.
With goals to establish medical necessity, ensure regulatory compliance, and enhance patient billing accuracy, hospitals can unlock benefits focused on precision, revenue, and efficiency.
This type of hospital admission software can also be seen as another form of clinical documentation improvement software – an advanced conduit to increase the accuracy, detail, and quality of medical information. A sound clinical documentation system aids in nourishing a healthcare facility’s financial health, reinforces compliance, and offers an honest reflection of patient care levels.
Essentially, these systems serve as authorities over medical necessity review software, ensuring every treatment, test, procedure, or drug correlates with a patient’s condition. They can significantly
-
- Decrease the likelihood of contraindications.
- Curtail the risk of readmissions.
- Keep overtreatment at bay.
- Lead to far better patient outcomes.
The largest gap in the Utilization Management process right now at most health systems is physician bed status determinations and documentation of medical necessity.
With the improvements AdmissionCare makes on these items, more patients will be in the appropriate bed status to begin with and have proper documentation.
This makes it so the Utilization Review team doesn’t have to spend half their day digging out of all of the admissions that came in overnight. UR staff can more time on complication admissions, concurrent reviews, and appeals letters.
Get a customized demo of AdmissionCare for your health system today!