Medical Necessity Documentation
Medical necessity documentation in the healthcare sector encompasses the process of recording and showing the cause for the need for medical services or treatments given to patients. This medical documentation is evidence to support the medical necessity of a given medical procedure, treatment, or hospital admission. Without proper documentation, healthcare providers may face challenges getting payments from health insurance companies. They can also be subject to financial audits if they do not know how to document medical necessity.
The provision of healthcare services must be appropriate, rational, and necessary given the patient’s diagnosis and condition, according to medical necessity documentation. It helps prove the suggested treatment plan’s medical necessity and confirms that it adheres to accepted medical standards and guidelines. Medical necessity documentation is also meant to protect patients. These documents forbid pointless procedures or treatments that could put patients at risk or put an unjustified financial strain on them.
Healthcare practitioners must include relevant and specific information in a patient’s medical records to prove medical necessity accurately. It should thoroughly account for the patient’s condition, symptoms, medical background, and prior treatments. These elements must be closely related to the suggested treatment, demonstrating the necessity of that treatment.
The variables for establishing the appropriateness of a specific medical intervention or hospital admission are recognized as medical necessity criteria. These criteria are often devised to address the issue of how to document medical necessity. Healthcare practitioners must become acquainted with these criteria and ensure their documentation meets the stipulated requirements.
Medical necessity documentation for hospital admissions is equally just as necessary. Healthcare professionals must record the patient’s medical condition, the seriousness of their symptoms, and whether or not they require inpatient care. They should also explain why outpatient care is not an option for that patient and offer alternative solutions. Healthcare providers boost their chances of reimbursing hospital stays by meeting the medical necessity criteria for specific hospital admissions and providing proper documentation.
But ask most admitting physicians, and they’ll tell you they didn’t learn about medical necessity criteria in school or their training, as it hasn’t historically been a physician-led initiative.
Provider Documentation Requirements
For efficient documentation of medical necessity, healthcare professionals must follow particular documentation guidelines. Specific criteria are in place to ensure thorough and accurate documentation, which is necessary for claiming compensation and adhering to the rules. What are the essential provider specifications for documenting medical necessity?
Clear Diagnosis
Healthcare providers must document their patient’s diagnoses accurately and clearly. It includes describing the patient’s condition, symptoms, and other relevant test results supporting the diagnosis. The documentation should support the medical necessity of the proposed medical service or treatment and establish a direct link between the diagnosis and the need for the specific service.
Justification for Treatment
Healthcare providers must justify the need for the proposed treatment or service for the patient’s care, following the provider documentation requirements. Based on the patient’s health and medical background, they ought to provide a thorough clinical justification. The progression of the patient’s illness and the necessity of ongoing therapy intervention are both explained by this information. Additionally, it enables a review of the patient’s response to earlier therapies, which can support the medical necessity of the suggested service even more.
Inpatient Hospital Admission Justification
Healthcare providers must provide documentation describing the need for inpatient care to meet hospital admission criteria based on medical necessity. It includes the extent of the patient’s disease, complications, and anticipated care. In addition, healthcare professionals must explain why outpatient treatment or substandard care will not be sufficient to meet the patient’s needs.
Compliant with Medical Necessity Criteria
Healthcare providers must ensure that their documentation meets the specific medical necessity documentation requirements that regulatory bodies and insurance companies set forth.
Relevant Medical History
Another Medicare documentation requirement is the patient’s relevant medical history. It should include previous treatments and their outcomes. The information on medical history helps establish the medical necessity of the current medical procedure.
Expected Outcomes
Provider requirements for medical documentation seek healthcare professionals to document the anticipated outcomes and goals of the treatment or service. It shows the potential benefits and positive impact on the patient’s health.
How To Ensure Medical Necessity Documentation Compliance
Complying with medical record documentation requirements is essential for healthcare providers to ensure accurate and compliant documentation. It enhances quality patient care, facilitates proper reimbursement, and helps maintain regulatory documentation compliance. Here are some basic steps on how to ensure medical necessity documentation compliance.
-
- Become Familiar with Medical Documentation Guidelines: Healthcare practitioners should become familiar with the guidelines and protocols for documentation and healthcare records that regulatory bodies have established for documentation and medical records. The conditions for proving medical necessity are outlined in these recommendations.
- Stay up-to-date with Changes: Health practitioners must stay informed about any updates or changes to the medical necessity documentation compliance requirements. They should regularly review the guidelines to ensure compliance with the latest standards and practices to ensure that they are complying with medical record documentation.
- Understand Medical Necessity Criteria: They should clearly understand the medical necessity criteria for different medical services or treatments hence achieving documentation compliance. In addition, they should be aware of the specific documentation elements required to demonstrate medical necessity in different clinical scenarios.
- Document Patient’s Condition: Medical documentation compliance requires healthcare providers to document their patients’ condition comprehensively. They must include all the relevant information, such as symptoms, physical findings, diagnostic test results, and the effect of the disease on the patient’s daily activities and general health.
- Justify Treatment Decisions: They must provide a clear and detailed clinical rationale for the chosen treatment or service. They further need to explain why it is necessary for the patient’s care and how it aligns with the medical necessity criteria. Finally, they must consider including supporting evidence or research to strengthen their justification.
- Include Relevant Medical History: Healthcare providers must incorporate their patient’s relevant medical history, including previous treatments and outcomes. This information provides context and supports the medical necessity of the current intervention.
Medical Necessity Denials
Medical necessity denials have become a growing concern for healthcare providers. It has dramatically contributed to financial challenges and increased administrative burdens. Medical necessity denials occur when insurance companies consider that the provided healthcare services or treatments are not medically necessary. The refusal results in non-payment or partial reimbursement for the care provided. Healthcare organizations are therefore forced to invest time and resources in medical necessity appeals to secure their rightful reimbursement.
One of the main reasons for the increase in medical necessity denials is the ever-changing regulations and documentation requirements. Insurance companies have strict guidelines for determining medical necessity. Any identified shortcomings in the documentation could lead to a denial. It usually happens even when medical services are necessary for the patient’s health and well-being.
To address this issue, healthcare providers must use proactive strategies to minimize medical necessity denials and streamline the appeals process. Investing in medical necessity training for all staff involved in the documentation and billing processes is essential. Through comprehensive training, healthcare professionals can better understand the specific medical necessity criteria for different services and treatments. They will also learn how to document medical necessity accurately and effectively, reducing the likelihood of denials due to documentation gaps.
A dedicated team handling medical necessity appeals can remarkably improve the chances of canceling denials. This team can carefully review denied claims, identify the reasons for denial, and gather the necessary evidence to support the medical necessity of the provided care. By presenting a strong and well-documented appeal, healthcare organizations can strengthen their case and increase the likelihood of successful reimbursement.
Healthcare providers can also benefit from proper medical necessity resources. These resources may include industry guidelines, best practices, and educational materials that give insights into navigating the complexities of medical necessity documentation and appeals. Staying informed and up-to-date with industry resources can empower providers to proactively address issues related to medical necessity and avoid potential denials.
Medical Necessity Software
In the fast-paced and data-driven world of healthcare, accurate and compliant medical necessity documentation is essential. In addition to following the above best practices, medical necessity software has emerged as an invaluable solution that helps healthcare providers get their documentation right at the source.
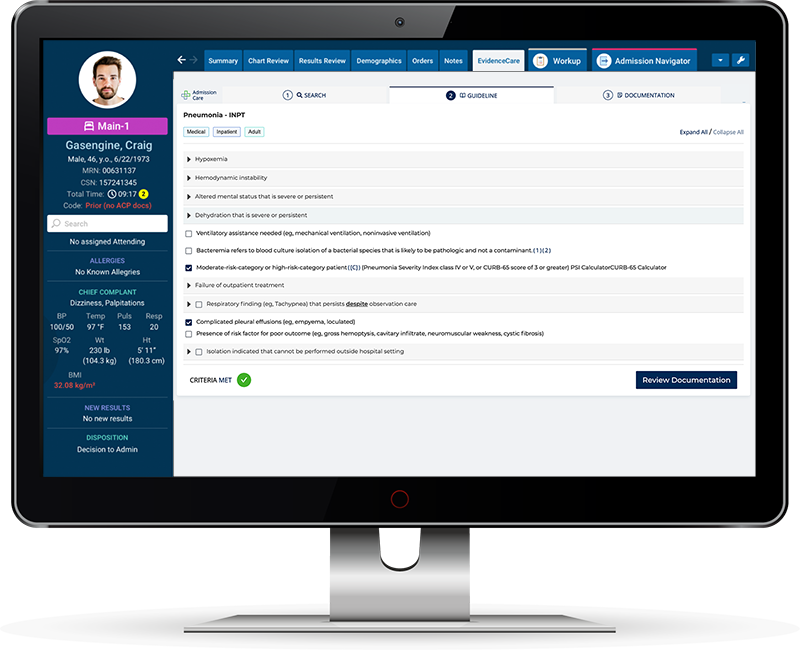
Medical necessity documentation software like AdmissionCare streamlines the documentation process, enhances efficiency, and ensures adherence to medical necessity criteria. There are a lot of medical necessity software options available today, but many are focused on post-care processes for utilization management and denial management teams.
Medical necessity documentation compliance software like AdmissionCare is a robust tool that assists admitting physicians in documenting medical necessity in the EHR at the point of care in line with the requirements set by companies such as MCG and Interqual. This software has features that prompt healthcare providers to include all essential information during the patient encounter. It guides them through the documentation, ensuring clinical details are noticed and included. It reduces the risk of medical necessity denials due to incomplete documentation.
To address the challenges particular to this setting, dedicated medical necessity documentation software for hospital admissions offers a personalized approach. These software programs record detailed patient information, such as their symptoms, diagnoses, and reasons for hospital admission. Medical necessity software facilitates a more logical and accurate portrayal of the patient’s medical condition, which is essential for proving the need for hospitalization by gathering all required data in one location.
The user-friendly, EHR-integrated interface of AdmissionCare make it easier for doctors to move through the documentation process quickly and efficiently. This improves clinical workflow and ensures that documentation is completed on time, reducing the likelihood of delays and re-work.
The fact that the medical necessity software has real-time guidance and integrations to help healthcare practitioners remain on top of their medical necessity documentation needs is a huge benefit.
Healthcare providers can improve their compliance with medical necessity documentation standards by employing medical necessity software. It lessens administrative work even more and enhances patient care in general. Medical necessity software will become increasingly important in the age of digital healthcare advancements, helping hospitals improve documentation procedures and fulfill their commitment to giving patients high-quality, well-documented care.
Contact EvidenceCare and start your healthcare facility’s journey to more streamlined medical documentation with AdmissionCare.
Schedule a customized demo of AdmissionCare today.