Revenue Cycle Management in Hospitals
The revenue cycle management process forms the backbone of any hospital’s financial operations. Efficient and streamlined revenue cycle management in hospitals ensures that patients’ bills are correctly handled, medical billing is accurate, and payments are collected promptly.
In simple terms, revenue cycle management in medical billing refers to all the financial steps hospitals take, from when a patient schedules an appointment to receiving treatment. It also involves steps patients follow when billed for services, obtaining an insurance claim response, and settling their accounts. Any disruption or inefficiency at any stage can drastically affect a hospital’s financial health.
Some examples of technologies used in revenue cycle management include:
-
- Electronic medical record (EMR) or electronic health record (EHR) systems
- Practice management software
- Patient engagement platforms
- Claim scrubbing software
- Automated billing systems
- Payment processing systems
- Analytics and reporting tools
One of the biggest challenges revenue cycle teams face is denial management. Insurance companies often deny or only partially approve medical claims due to coding issues, lack of required documentation, eligibility errors, or other reasons. This results in unpaid bills, which hospital revenue cycle management teams must investigate and resubmit. The lengthy denial management process and denial management workflow lead to delays in payments and erosion of revenue.
These are some strategies to reduce hospital denials, including:
-
- Train staff on proper coding, documentation, and billing procedures to ensure accurate and complete claims
- Review denied claims thoroughly to identify coding, documentation, or billing issues that led to the denials
- Improve communication between clinicians, utilization review, coders, and billers
- Utilize clinical decision support tools and health IT systems that can flag potential issues during documentation to minimize errors before claims are submitted
- Conduct regular audits of claims and encounters to proactively identify issues that could lead to denials before they happen
- Ensure patients have verified insurance eligibility and coverage details before services
Hospitals employ sophisticated clinical revenue cycle management technologies that address denial issues at the source using automation, data analytics, and machine learning. Such technology optimizes billing, follows up with payers, identifies leakage areas, and minimizes payment denials. Implementing robust revenue cycle management healthcare and denial management systems has become critical to a hospital’s financial viability in today’s complex healthcare landscape.
Steps of Revenue Cycle Management
The revenue cycle in healthcare involves several stages and requires effective management to ensure financial success. It is a strategic approach taken by healthcare organizations to optimize the revenue cycle management process and achieve financial stability.
Let’s delve into the detailed steps in the revenue cycle:
-
- Patient Scheduling and Registration: The healthcare revenue cycle steps commence with scheduling patient appointments. It involves verifying patient insurance coverage, gathering demographic and insurance information, and scheduling appointments based on availability and medical necessity. Patients provide personal and insurance information during the registration process and the data used for accurate billing and reimbursement.
- Coding and Charge Capture: In this step of revenue cycle management, healthcare services and procedures provided to patients are documented using medical codes (such as CPT and ICD codes).
- Claim Submission: Once coding and charge capture are complete, claims are generated and submitted to the appropriate insurance providers. This critical step includes preparing and electronically transmitting claims.
- Claims Processing: After claim submission, insurance providers review the claims and determine payment amounts based on coverage and contract agreements.
- Payment Posting: Once claims are processed, payments from insurance companies, patients, and third-party payers are received. Accurately recording payments, adjustments, and denials in the financial system is essential
- Denial Management: Denials are common in the revenue cycle and can impact financial performance. This stage includes analyzing denial reasons, appealing denied claims when appropriate, and implementing strategies to reduce future denials.
- Patient Billing and Collections: Patient billing is integral to revenue cycle management. It involves generating patient statements, explaining charges, and providing payment options.
- Reporting and Analysis: Monitoring and analyzing revenue cycle performance are crucial for identifying areas of improvement and making strategic decisions. This stage includes generating financial reports, analyzing key performance indicators (KPIs), and implementing process enhancements based on data-driven insights.
By following these steps of revenue cycle management, healthcare organizations can streamline their financial operations, optimize reimbursement, and achieve financial stability. Effective revenue cycle management ensures improved cash flow and financial success and allows healthcare providers to focus on delivering quality patient care.
For instance, efficient RCM processes ensure patient bills are generated promptly and accurately. According to a survey by the Medical Group Management Association (MGMA), practices with effective RCM systems experience a median decrease in accounts receivable (AR) days of 5.5%, indicating faster billing and collection processes.
An American Medical Association (AMA) study also estimated that medical practices could save up to 15% of their total costs by implementing effective RCM practices.
Revenue Cycle Management Companies
Revenue cycle management companies play an integral role in the healthcare industry. They optimize revenue cycle management processes to maximize revenue, efficiency, and reimbursements for hospitals and physician practices.
Healthcare revenue cycle management companies utilize advanced technologies, analytics, and personnel to improve every step of the revenue cycle, from patient access and registration through claims processing and collections. They automate workflows, standardize processes, and monitor performance metrics. That way, revenue cycle management healthcare companies help providers increase cash collections, reduce denied claims and administrative expenses, and comply with complex billing regulations.
The top RCM companies active in the healthcare industry include:
-
- EvidenceCare: This revenue cycle management company is unique as it focuses on clinical decision support software that prevents many of the issues that plague revenue cycle teams. EvidenceCare is considered complementary to many of the outsourced revenue cycle services available in the market but has proven to reduce denials, secondary level reviews, and the administrative burden on physicians and UR staff that cost hospitals so much time and money. EvidenceCare’s pricing structure is designed to deliver value-based results, aiming to improve margins by increasing revenue and reducing costs for health systems.
- Optum: One of the largest revenue cycle management firms, Optum manages the revenue cycle for over 1,300 hospitals and health systems. Their pricing structure may vary depending on factors such as the size of the healthcare organization, the range of services required, and the complexity of the revenue cycle management needs.
- Change Healthcare: Change is also among the top healthcare revenue cycle management companies. Change managed over $660 billion in medical claims payments in 2018. Change Healthcare charges a mix of percentage, per-claim, and per-head fees.
- R1 RCM: R1 provides end-to-end revenue cycle management solutions, including patient access, claims processing, and payment integrity management. R1 RCM utilizes a revenue-sharing model where they charge a reduced management fee but also receive a percentage of the incremental revenue they generate for clients.
- Ensemble Health Partners: One of the largest healthcare revenue cycle management companies, Ensemble specializes in outsourced revenue cycle solutions and technologies with experienced operators. They do everything from acute assessments to targeted ROI solutions to a fully outsource revenue cycle department.
Innovative Revenue Cycle
Healthcare organizations are constantly looking for ways to streamline and optimize their revenue cycles to reduce costs and improve cash flow. New technologies and innovative clinical-driven solutions offer opportunities to transform the revenue cycle in impactful ways.
Here are some examples of technologies and solutions used in the industry:
-
- Automation and AI tools: Adopting automation and artificial intelligence tools to eliminate manual tasks and errors. This includes charge capture software that pulls charges from EHRs, insurance eligibility verification platforms, and claims routing systems with business rules engines. Automated denial management can resubmit claims promptly.
- Utilization Review tools: Using utilization review and utilization management technologies to reduce unnecessary procedures and costs while maintaining outcomes. Data analytics platforms can identify high-risk patients, high-cost interventions, and standardized care opportunities.
- Automated charge capture from EHRs: Healthcare organizations implement tools that automatically extract charge information from Electronic Health Records (EHRs). This technology reduces manual effort and minimizes errors in the revenue cycle management process.
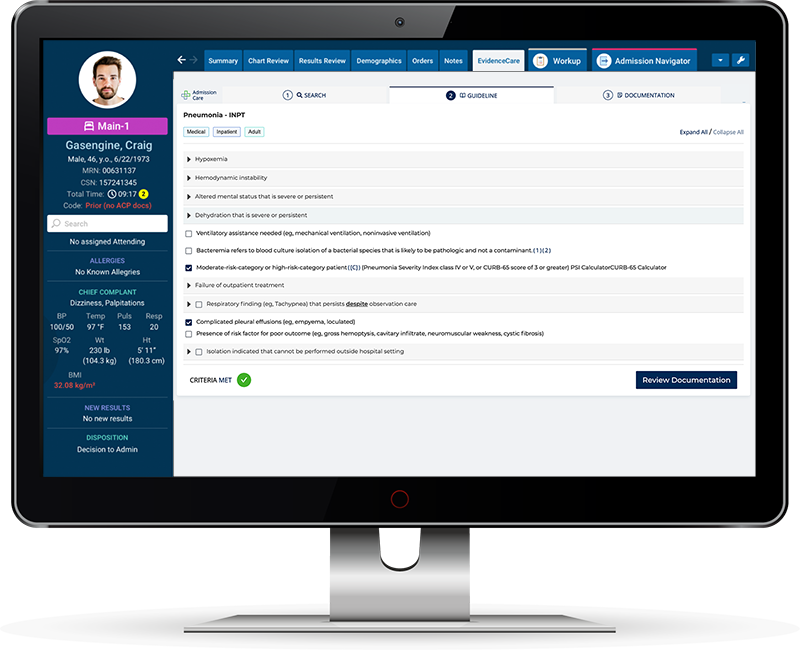
- Integration of clinical guideline support: Solutions such as EvidenceCare directly integrate clinical guidelines and evidence-based support into provider workflows. This technology assists providers in making informed decisions at the point of care, ensuring compliance with utilization and documentation standards, ultimately leading to proper billing practices.
- Automation of patient communications: Healthcare organizations are automating patient communications to improve the patient experience and streamline collections and customer service efforts. It includes implementing chatbots, texting services, and interactive voice response systems to enhance patient engagement and increase collection yields.
Revenue Cycle Management Software
Revenue cycle management software helps streamline the process of billing patients quickly and accurately, reduce costs, and maximize reimbursements. Hospitals depend on revenue cycle management software to maintain profit margins with rising healthcare costs and declining reimbursements.
These are some of the features and functionalities that hospitals should look for when selecting a software solution:
-
- Electronic Health Record (EHR) management: Efficiently manage and store patient medical records electronically
- Clinical decision support: Provide alerts, reminders, and evidence-based guidelines to aid clinical decision-making
- Interoperability: Enable seamless sharing of patient information across different systems and healthcare providers
- Billing and revenue cycle management: Streamline coding, claims submission, and payment processing for efficient financial management
- Medication management: Support electronic prescribing, medication reconciliation, and drug interaction checking to enhance patient safety
Traditionally, many RCM functions have been managed manually through paper forms, spreadsheets, and stand-alone software applications. However, denial management software that unifies all revenue cycle functions into one integrated platform can lead to improved outcomes.
In addition to core revenue cycle features, hospitals should look for software that incorporates clinical tools for the revenue cycle. For instance, tools that help physicians get the appropriate hospital admission criteria and correct documentation upfront can significantly reduce denials from payers and rework by utilization review.
An example is EvidenceCare’s AdmissionCare, a clinical documentation tool for physicians during patient admissions. Though primarily a clinical tool, AdmissionCare helps the revenue cycle by reducing the utilization management burden on physicians and reducing medical necessity denials.
For more information on how AdmissionCare can help your revenue cycle, schedule a customized demo.