Hospital Admission Documentation Requirements
Comprehensive, accurate hospital admission documentation requirements are critical in healthcare. In light of growing denial issues and the rapid pace of emergency departments, maintaining meticulous hospital admission documentation has never been more important. Doing so helps streamline hospital processes and ensure continuity of care.
Hospital admission documentation is a decisive factor that pairs the patient’s condition with the appropriate treatment. Proper documentation outlines the rationale for the admission, linking the patient’s clinical needs with the prescribed diagnostic or therapeutic measures. This process contributes to effectively mobilizing resources, enhancing the quality of patient care, and improving hospital efficiency.
Diving deeper into clinical documentation, you’ll find that it’s foundational to any hospital’s mission. It includes elements like:
-
- Medical history
- Clinical findings
- Diagnostic test results
- Medication orders
The detailed nature of clinical documentation provides complete transparency into the patient’s treatment journey, fortifying trust between the healthcare provider and the recipient. However, the importance of documentation in healthcare extends beyond simple record-keeping. It can become a powerful tool that showcases the hospital’s effectiveness and compliance with healthcare regulations. And as many revenue cycle and utilization review leaders will tell you, documenting medical necessity for hospital admissions is crucial for hospitals getting reimbursed by payers.
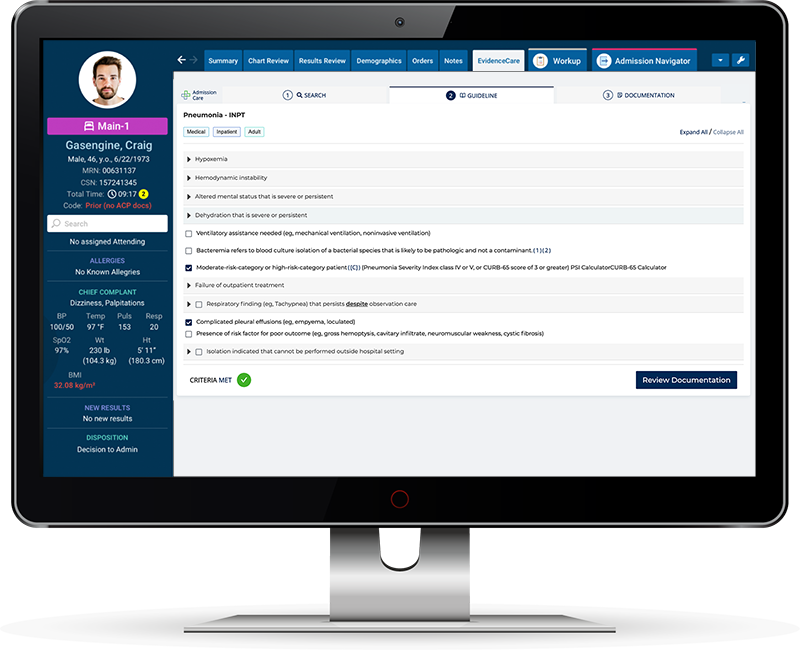
Good documentation practices often lead to fewer audits, fewer claim denials, and an enhanced reputation, key ingredients to ensuring the hospital’s sustainability in a fiercely competitive healthcare sector. Technology like EvidenceCare’s AdmissionCare software helps healthcare professionals navigate the complexities of hospital admission documentation requirements. It can also help hospitals use resources more efficiently, resulting in cost optimization and more efficient patient care.
These tools can transform the documentation process into a seamless, effortlessly manageable task, embodying the ideals of efficacy and precision intrinsic to the healthcare sector.
Key Components of Hospital Admission Documentation
Hospital admission documentation is a comprehensive process that involves several components you need for appropriate patient care and streamlining admissions. Some of these critical elements include:
-
- Criteria for hospital admission
- Documentation within medical records
- Inpatient vs. observation criteria
- Medical necessity documentation
While the type of criteria used for hospital admissions may vary from one institution to another, they rely fundamentally on two cornerstones: the medical necessity for inpatient services and the doctor’s certification for the necessity of admission.
Medical necessity refers to the requirement for a particular set of health services that a physician decides are necessary to treat the patient’s illness or injury.
The quality and specificity of documentation within medical records are paramount to realizing beneficial patient outcomes and maintaining effective hospital management. These records must include comprehensive patient information such as medical history, diagnostic tests, proposed treatment plans, and medication orders.
Proper documentation, serving as the primary mode of communication among healthcare providers, helps to build continuity in patient care by enabling a smooth transition between different service providers. Defining the course of a patient’s stay in the hospital isn’t a straightforward process; it often hinges on the stark difference between inpatient admission criteria and observation criteria.
The decision between the two often hinges on the severity of the patient’s condition, the need for complex medical equipment or round-the-clock care, or the necessity for a surgery that requires a recovery period in the hospital. Therefore, along with medical need, the decision to admit someone as an inpatient or keep a current patient under observation significantly impacts the hospital length of stay, which is another critical area tracked for improving the operational efficiency of a hospital system.
Meanwhile, medical necessity documentation plays a crucial role as it supports the required services rendered, thereby ensuring their appropriateness, reducing the risk of denials, enhances communication, and justifies the length of hospital stay. The process typically includes documenting symptoms, diagnosis, the risk of the current condition, the potential benefit of hospital services, and proof of delivery of these services. In conclusion, accurate and thorough hospital admission documentation is not just fundamental for effective patient care, but also serves as a pivotal tool for hospitals to maximize their clinical outcomes and operational efficacy.
The criteria for hospital admission, inpatient admission versus observation status, and medical necessity documentation are all key aspects of this process. These elements, collectively, streamline the functioning of the hospital system, ensure seamless communication among healthcare providers, and result in a well-coordinated patient care delivery plan.
Regulatory Requirements and Standards
Understanding the precise regulatory requirements and standards established for hospital admissions is paramount for hospital clinicians. These criteria and guidelines are an imperative part of the documentation process, which aids in ensuring that patients receive the most appropriate level of care. The ways in which these regulatory measures, such as clinical decision unit admission criteria, emergency department documentation requirements, CMS medical record documentation requirements, contribute to health information management is multifold.
The Clinical Decision Unit (CDU) admission criteria essentially guide the admission process, providing a structure that ensures only those needing specific standards of care are admitted to a CDU. Through these criteria, physicians and healthcare providers make well-informed decisions on patient care, minimizing risks and maximizing the likelihood of successful treatment.
In parallel with the CDU admission criteria, Emergency Department Documentation Requirements (EDDR) serve an equally vital role. Tasked with saving lives within an environment that is rapid-paced and often chaotic, efficiency and accuracy are of the essence in the emergency department. EDDR mandate that healthcare providers produce a detailed and accurate account of patient encounters to enhance patient care, provide legal protection for the physician, facilitate effective communication among health team members, and aid billing processes.
Furthermore, within the spectrum of regulatory requirements and standards, the CMS medical record documentation requirements act as a directive for providers, dictating the precise standards required for recording and managing health information for Medicare reimbursement. Compliance with these requirements ensures the integrity of the data and provides a valuable resource for use in clinical decision-making and continuity of care.
Understanding CMS’s “two midnight rule” and using it correctly is a pivotal factor in hospital admissions, particularly when it comes to patient classification. This rule delineates the criteria by which a patient is considered an inpatient or under observation status. Knowing the fine line between these statuses is beneficial from a medical standpoint and a financial perspective, primarily because different reimbursements come with different statuses.
These regulatory standards and requirements collaborate for effective health information management. They dictate how data is recorded, stored, and used within healthcare settings, offering a guide to ensuring best patient outcomes and streamlining organizational operations.
The Medicare inpatient admission criteria also play a significant role in regulatory requirements and standards. These guidelines set the bar for the quality of care expected for medicare beneficiaries and lay the foundation for the regulations applicable to all patients, ensuring an efficient, effective, and equitable health system. When adhered to meticulously, the culmination of these standards serves the dual purpose of ensuring patient safety while enabling the smooth operation of healthcare organizations.
Hospital Admission Documentation Best Practices
Systems such as EvidenceCare’s AdmissionCare have revolutionized hospital admission documentation practices. The software gives physicians the admission criteria and medical necessity documentation required to easily choose between inpatient and observation status. This process takes place at the point of care and is integrated within the EHR (Electronic Health Record) system. Crucially, this innovation results in extensive resource and capital savings by preventing clinical interruptions and insurance claim denials rooted in inadequate documentation.
The importance of documentation standards in the electronic health record cannot be overstated. Adequate, accurate, and timely documentation:
-
- Ensures exceptional patient care
- Enhances healthcare providers’ communication
- Supports clinical decision-making
- Facilitates billing and reimbursement processes
An effectively implemented EHR system – enhanced by integrated CDS – is foundational to a functional health system because it helps implement documentation standards and improves overall operational efficiencies. A central pillar of quality improvement in hospitals is the optimization of medical documentation guidelines. Accurate, complete medical records ensure the delivery of high-quality, patient-centered care. Moreover, they safeguard hospitals from legal issues that may arise from deficiencies or inaccuracies in medical records.
Medical documentation guidelines are a protective shield that strengthens the hospital’s defense mechanism against potential clinical and financial risks. The digitization of healthcare records and improved electronic medical record documentation created an era of unprecedented data accuracy and accessibility. Just by pressing a few keys, physicians can consult comprehensive patient records – a task that would have demanded hours in the past. This ease of access facilitates quicker, more accurate diagnoses and superior patient outcomes. However, transitioning to a digital documentation system presents some challenges.
Successfully incorporating electronic records into a healthcare institution demands a systemic change. Simply training staff to use the system isn’t enough because you must also update underlying processes and procedures. Investing in hospital admission documentation best practices, such as admission criteria software, rigorous physician training, and regular documentation audits, can help mitigate these challenges.
These practices heighten the documentation process’s accuracy and promote trust and collaboration among clinicians. As a result, patients receive higher-quality care, and hospitals see dramatic improvements in operational efficiencies, cost savings, and increased earned revenue.
Superior digital documentation processes, such as those championed by EvidenceCare’s AdmissionCare, can transform the future of healthcare. By implementing rigorous documentation standards within electronic health records, embracing medical documentation guidelines, and introducing quality improvement measures, we can aspire to provide unparalleled patient care in a world where excellence is the new normal.
Schedule a customized demo of AdmissionCare today.